Blood in a Canadian Armed Forces Theatre of Operations
Warrant Officer Jeff Scott, BSc, MLT
Canadian Armed Forces Blood Program
Massive hemorrhage is the leading cause of potentially survivable death on the battlefield (1). The North Atlantic Treaty Organization (NATO) Allied Joint Medical Doctrine (2) has outlined expected medical care timelines for casualties in a theatre of operations using the 10-1-2 standard:
a. 10 minutes: Trained military personnel in Tactical Combat Casualty Care to provide immediate life saving measures;
b. 1 hour – Damage Control Resuscitation (DCR) initiated to restore homeostasis and prevent coagulopathy, hypothermia, and acidosis often with aggressive hemostatic resuscitation; and
c. 2 hours – Damage Control Surgery (DCS) to focus on surgical interventions to those with life threatening injuries (3).
In order to meet the one hour DCR standard, it is imperative that blood products are available pre-hospital in case medical evacuation from the point of injury to a medical treatment facility is delayed or unavailable. From a laboratory perspective, there are numerous challenges and considerations with respect to managing blood products in a deployed setting, namely cold chain and inventory.
The process of maintaining the appropriate temperature of blood products, no matter the location is the Cold Chain. This is achieved by employing passive temperature controlled devices (coolers) or active temperature controlled devices (portable refrigerators or freezers). Advance planning needs to be employed to ensure that cold chain can be maintained in uncertain or adverse conditions. Without sustainable cold chain, blood products would be unavailable when needed most.
Another challenge is maintaining an inventory of blood products in theatre. The Canadian Forces Health Services’ (CFHS) mandate is to ensure CAF members receive the same full-spectrum high quality health care abroad as they would in Canada (4). One of the biggest differences in a deployed theatre of operations compared to a civilian hospital in Canada is the availability of platelets. The short shelf life of platelets makes them logistically impractical to maintain in a deployed setting. This limiting factor means that due consideration needs to be made on deployments for the scope of care that can be provided.
The CFHS has identified whole blood as the preferred hemostatic agent for traumatic hemorrhage. Whole blood is never fractionated into its components; it contains all required components and is the only source of platelets available in an austere environment. Whole blood provides blood to the casualty in the same ratio that it’s lost. Deploying CAF members can volunteer to be pre-screened by Canadian Blood Services for potential fresh whole blood donation in a theatre of operations. The member undergoes the same donor qualification process as a civilian donating blood, but does not donate the unit of blood at the time of screening. If eligible, they donate whole blood when the need for whole blood arises while in theatre. This practice of collecting pre-screened fresh whole blood for a named patient in theatre is termed an Emergency Donor Panel (EDP).
Cold chain and inventory management are just a couple of the unique challenges and considerations with providing full spectrum health care in a deployed setting. An EDP is unique to the military environment and plays an extremely important role in providing lifesaving blood products.
- Eastridge BJ. Death on the battlefield (2001-2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012 Dec;73(6 Suppl 5):S431-7. doi: 10.1097/TA.0b013e3182755dcc. Erratum in: J Trauma Acute Care Surg. 2013 Feb;74(2):706. Kotwal, Russell S [corrected to Kotwal, Russ S]. PMID: 23192066.
- North Atlantic Treaty Organization. Allied Joint Publication 4–10(A) Allied Joint Medical Doctrine. 2011.
- Fisher, Andrew D. “Damage Control Resuscitation (DCR) in Prolonged Field Care (PFC) (CPG ID:73).” Joint Trauma System Clinical Practice Guideline (JTS CPG), 1 Oct. 2018.
- (The Canadian Forces Health Services (CFHS) Overview)
Announcement
Tech Assessment
The Tech Assessment program, Basic, Advanced and Dispensary Site will be launching in November 2022!
Featured Resources
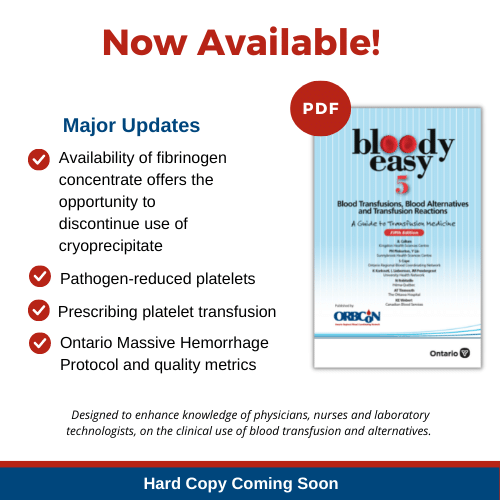
Bloody Easy 5
Purolator Healthcare Indicators

The Plasma Protein and Related Products (PPRP) redistribution program is adding the use of Purolator Healthcare Indicator labels in order to further identify our shipments as Healthcare/Hospital related and to avoid possible delays in redistribution of PPRP shipments. Notification and implementation for the use of the labels on the J82, E38 and MTS EMT shipping containers was sent on October 24th.
Updates to the following documents in our Redistribution Toolkit have been made to reflect this change:
- IM.006 – Shipping Blood Components Using the J82 & E38-Shipping Containers
- IM.011 – Shipping Blood Components/Products Using MTS Shipping Containers
- Shipping Blood Components and Products Training Checklist
Changes to the following documents will follow soon:
- Redistribution Hospital User Guide: Plasma Protein and Related Products Redistribution Hospital User Guide
- Narrated PowerPoint: Plasma Protein and Related Products (PPRP) Online Reporting Training Video
For questions or concerns please contact one of your ORBCoN or FCRP coordinators.
Dispensary and administration toolkit
ORBCoN has created a set of tools that can help the Dispensary/Administration sites design and implement a transfusion program. These tools include:
- A list of relevant Accreditation Canada Diagnostics Requirement
- Policy and Procedure Checklist
- Resource Checklist
- Power Point Presentation – Dispensary and Administration Site Information
- Memorandum of Understanding Template
If you have any questions about setting up an administration site, please reach out at transfusionontario@gmail.com
Upcoming Events
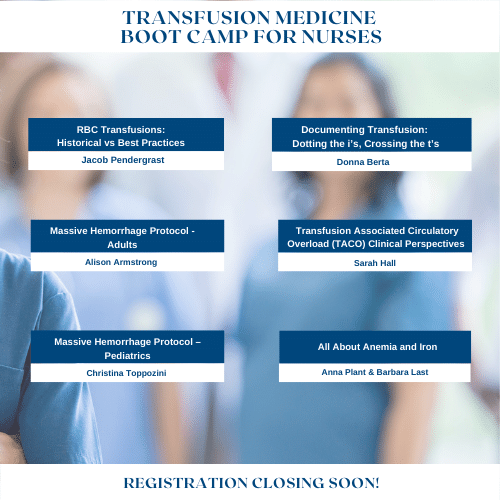
Transfusion Medicine Boot Camp for Nurses
Join these speakers for this year’s Transfusion Medicine Boot Camp for Nurses, Nov 23rd
Upcoming UofT TM Round

November 24, 2022 @12pm-1pm
MLT Session – Interesting Serology Cases
Virtual Session Only