Transfusion Related Roles for Nursing Officers
Maj Amy Godwin, RN
Blood Program Manager
Canadian Armed Forces
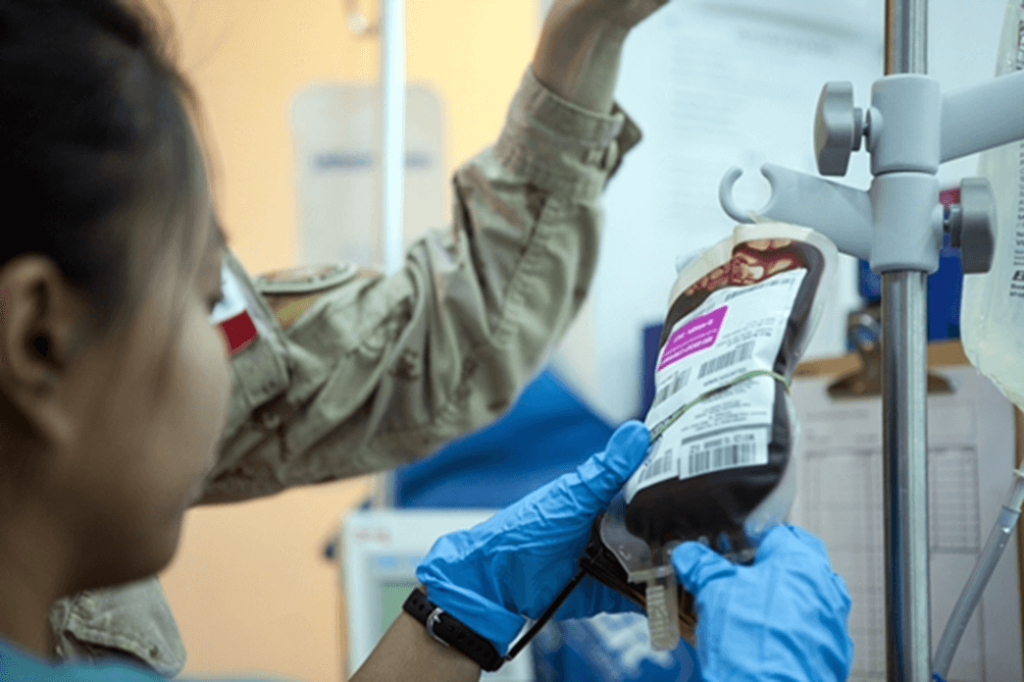
Canadian Armed Forces Nursing Officers are licensed Registered Nurses employed in various domains of nursing including direct patient care, clinical training, personnel management and strategic policy. A few of the specialities within the direct patient care domain include Medical-Surgical, Critical Care, Operating Room and Aeromedical Evacuation. Within each of these specialties, Nursing Officers may be called upon to fill blood management and transfusion roles.
To achieve clinical readiness for deployed missions, Nursing Officers receive trauma training to prepare them for roles in Damage Control Resuscitation (DCR). This training, amongst many other topics, includes familiarization with blood and blood products, Massive Hemorrhage Protocols and transfusion principles. Additionally, select Nursing Officers are designated as Blood Management Nurses and receive specialized training to lead the collection of fresh whole blood (FWB) in a deployed setting.
Despite detailed analysis and planning, circumstances may arise in deployed medical facilities where clinical demand for blood and blood products surpasses available resources and resupply timelines. In these extremis situations, FWB collected in theatre from a pre-screened volunteer donor offers an additional clinical capability towards the goal of life saving resuscitation. Once collected, FWB remains at room temperature for up to 24 hours prior to refrigeration and is not separated into components.
A deployed Nursing Officer assigned as the Blood Management Nurse will move from their primary duties to this role when an order is received to initiate screening for FWB. The Nurse assembles their team and commences recalling of pre-screened donors. Pre-screened donors are tested in Canada prior to a deployment by Canadian Blood Services and must meet the same eligibility criteria as any other Canadian blood donor. This stringent screening ensures FWB collected in a deployed setting is as safe as possible for immediate transfusion.
Once the donor is recalled to the medical facility, the Nurse and team complete another screening assessment including verbal attestations and collection of blood samples for testing by the lab. Upon receipt of lab results, the Senior Medical Authority decides whether a unit of blood is to be collected from the donor. The Blood Management Nurse is responsible for collection of the unit and documentation throughout the process. The lab then takes over responsibility of issuing the FWB unit to the trauma team for transfusion to a casualty.
FWB is most often collected during mass casualty events, meaning the facility is being overwhelmed and stretched beyond its capacity limits. The Blood Management Nurse needs to rely on their extensive training prior to the deployment to remain calm and deliberate while leading their team through the FWB collection process, most likely concurrently collecting from multiple donors. Errors made during the screening and collection phase could result in transfusion related reactions, including death. Training, ongoing practice and standardized approaches are used to minimize the potential for errors, in addition to the selection of a Nursing Officer with appropriate experience and skills to fill the vital Blood Management role.
Nursing in the CAF is an exciting job that offers unique clinical opportunities. The recruiting doors are open! Please reach out to Maj Godwin (AMY.GODWIN@forces.gc.ca) if you’re interested in learning more.
Announcement
Tech Assessment
The Tech Assessment program, Basic, Advanced and Dispensary Site will be launching in November 2022!
Featured Resources
Bloody Easy 5
Purolator Healthcare Indicators

The Plasma Protein and Related Products (PPRP) redistribution program is adding the use of Purolator Healthcare Indicator labels in order to further identify our shipments as Healthcare/Hospital related and to avoid possible delays in redistribution of PPRP shipments. Notification and implementation for the use of the labels on the J82, E38 and MTS EMT shipping containers was sent on October 24th.
Updates to the following documents in our Redistribution Toolkit have been made to reflect this change:
- IM.006 – Shipping Blood Components Using the J82 & E38-Shipping Containers
- IM.011 – Shipping Blood Components/Products Using MTS Shipping Containers
- Shipping Blood Components and Products Training Checklist
Changes to the following documents will follow soon:
- Redistribution Hospital User Guide: Plasma Protein and Related Products Redistribution Hospital User Guide
- Narrated PowerPoint: Plasma Protein and Related Products (PPRP) Online Reporting Training Video
For questions or concerns please contact one of your ORBCoN or FCRP coordinators.
Dispensary and administration toolkit
ORBCoN has created a set of tools that can help the Dispensary/Administration sites design and implement a transfusion program. These tools include:
- A list of relevant Accreditation Canada Diagnostics Requirement
- Policy and Procedure Checklist
- Resource Checklist
- Power Point Presentation – Dispensary and Administration Site Information
- Memorandum of Understanding Template
If you have any questions about setting up an administration site, please reach out at transfusionontario@gmail.com
Upcoming Events
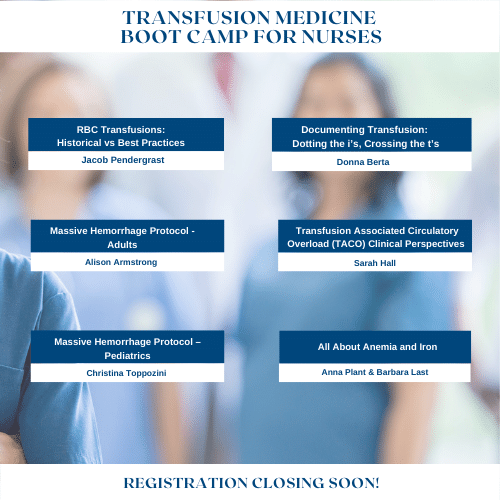
Transfusion Medicine Boot Camp for Nurses
Join these speakers for this year’s Transfusion Medicine Boot Camp for Nurses, Nov 23rd
Upcoming UofT TM Round

November 24, 2022 @12pm-1pm
MLT Session – Interesting Serology Cases
Virtual Session Only