Experience of MHP Implementation in 16 small rural hospitals
Dr. J. Radigan, FRCPC, Pam Vansteelandt, MLT, BSc., CLQM, MBA, Tasha Vandervliet, RN, BScN, Deanna Wright MBA, BSc, MRT(T)
Stratford General Hospital-Interhospital Laboratory program, Stratford, ON
The Interhospital Laboratory Partnership (IHLP) is a lab-partnership of 16 small, rural community hospitals in Southwestern Ontario. We have one blood bank hub site that does antibody identification, 8 sites that do basic blood banking and crossmatching, and 7 dispensary sites which only carry emergency O PRBCs onsite.
Since the release of the MHP Toolkit in 2020, we have been transitioning from a lab-based Massive Transfusion Procedure to a Hospital-based Protocol. After some delays due to COVID and Health-human resource shortages, our sites have been either refining existing processes, or actively developing their Hospital/Alliance-specific MHPs.
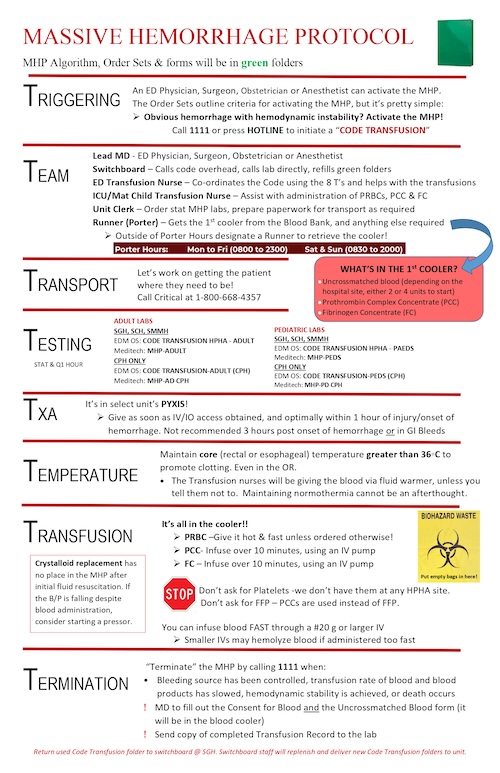
A multidisciplinary team including nursing, nurse educators, lab staff, pharmacy, and maintenance have contributed their expertise and experience to make implementation successful. We have utilized the resources from the provincial MHPs. We have utilized the resources from the provincial MHP toolkit, and have attempted to optimize plans for unique local conditions. Small rural sites have specific challenges that were not clearly addressed in the MHP Toolkit such as, the types and quantity of blood products available on site, staffing levels, and availability of transport.
Given the limited lab staffing at rural sites, we have opted to utilize prothrombin complex concentrates (PCC), instead of plasma. This enables nursing to remove the product from the lab and reconstitute; avoiding ABO incompatibility issues, thawing requirements and product ratio tracking. For similar reasons, we have also implemented the use of fibrinogen concentrate (FC) across the region as a replacement for cryoprecipitate.
To validate the proposed MHP processes before finalizing them, Mock Code Transfusions were held in various rural EDs and key care areas. This not only garnered stakeholder buy-in but also enabled the multidisciplinary team to assess necessary process changes at each level to align with protocol goals. These simulations underscored the importance of prioritizing transfers to larger centers and provided valuable practice opportunities for nursing staff in reconstituting and administering PCCs and FCs, as well as utilizing blood warmers and warming blankets.
Physician education is continuous. Given the diverse care provided by our medical staff, training for less common protocols competes with other priorities. The MHP undergoes review by the Medical Advisory Committee before approval. Transfusion training is integrated into Grand Rounds and other educational opportunities for medical staff.
We have been successful in consistent early administration of Tranexamic acid (TXA). We have recently involved local paramedics, with the objective to incorporate pre-hospital TXA administration, where possible.
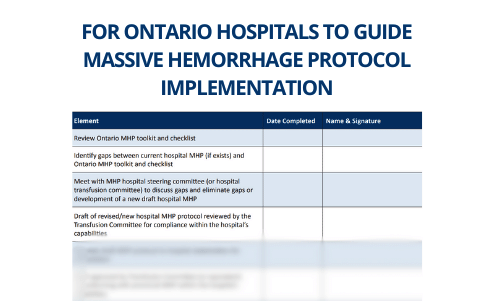
Knowing the expectation for quality metrics has been helpful in the process, thus we took the approach of evaluating MHPs in terms of these quality metrics. Quality data will be useful in both process improvement and optimizing future blood product inventory levels.
With guidance and data provided by ORBCoN and CBS, we envision walking this fine line of balancing responsible resource management while still ensuring effective MHPs at all our rural hospital sites.
Featured Resources
19th Annual TM Education Web Symposium
Ontario’s MHP: Guidance for small/remote hospitals
Implementation Checklist (MHP Toolkit) – Adult
Patient Transport (MHP Toolkit)
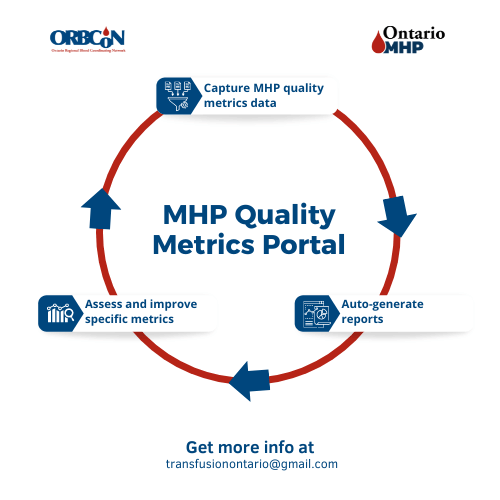
MHP Quality Metrics Portal
Note: Each Ontario hospital will need to determine where the data for the metrics is housed within their facility and who will be responsible for gathering and entering the data.
Upcoming Events
Transfusionists Talk
CSTM 2024

U of T

June 20, 2024 @12pm-1pm
MLT Session – Interesting serology cases
Subscribe to U of T Transfusion Medicine Rounds mailing list to get registration details