Massive Hemorrhage Protocol Implementation at Small Hospitals: Challenges, Possible Solutions, and Opportunities
Talal Mahdi, MD, FRCPC
Hematopathologist, Eastern Ontario Regional Laboratory Association, The Ottawa Hospital
Massive hemorrhage protocols (MHPs) are vital tools designed to expedite the provision of blood components in emergent situations based on best practices for the management of massively bleeding patients. These best practices include early identification of the massively bleeding patient, rapid provision of blood components and products, and a coordinated human resource response aimed at rapid identification of and control of bleeding.
While all hospitals that contain emergency departments, operating rooms, and/or obstetrical services should have MHPs, there are certainly challenges that may come with their implementation. These can include engaging and educating clinical partners, staffing limitations, limited inventories of blood components and products, limited laboratory test variety, and the ability, or rather, the inability to offer definitive hemorrhage control. However, amidst these obstacles lie potential solutions to optimize MHP implementation and efficacy, and ultimately, improve patient care.
Potentially the most significant obstacle to effective MHP implementation at small hospitals is the engagement and education of clinical colleagues. It is crucial that all individuals involved in carrying out the MHPs are engaged throughout the process, and all educated to be on the same page, as the MHPs require a rapid, coordinated team response. This can be done through the creation of specialized subcommittees as well as holding regular education and review sessions for all those who may be involved in the implementation.
At the heart of MHP efficacy lies the timely identification of massively bleeding patients and the rapid provision of necessary blood components or products. However, staffing limitations pose a significant hurdle in this process. To address this, hospitals can implement after-hours working policies and procedures. By empowering physicians and nurses to obtain blood units with appropriate documentation outside regular hours, hospitals can bolster their ability to respond promptly to hemorrhage cases.
Moreover, tailoring blood tests to match available resources during after-hours shifts can further streamline the process. Utilizing point-of-care instruments for this allows for efficient testing, enabling swift decision-making regarding blood component provision.
If patient transfer is necessary, proactively preparing for such events can be accomplished by establishing clear criteria for MHP activation. Additionally, due to the scarcity of MHP activation in most centers, running regular mock MHP activities can help maintain staff competency and ensure readiness to execute protocols effectively when the need arises.
Retrospective learning is a valuable tool as well, and implementing regular audits provides valuable insights from previous MHP activations, facilitating compliance with regulations and driving continuous quality improvement.
Lastly, when faced with unavoidable blood components and product inventory limitations, it is important to foster communication and collaboration with nearby hospitals. This can bolster support during blood component and product shortages and patient transfers, forming a network of assistance in times of need.
While challenges in implementing MHPs persist, proactive measures and innovative strategies offer pathways to surmount these obstacles. By leveraging adaptive solutions, maintaining a network of support with one another, and fostering a culture of continuous improvement, hospitals can enhance their capacity to respond swiftly and effectively to cases of massive hemorrhage, ultimately improving patient care.
Featured Resources
19th Annual TM Education Web Symposium
Ontario’s MHP: Guidance for small/remote hospitals
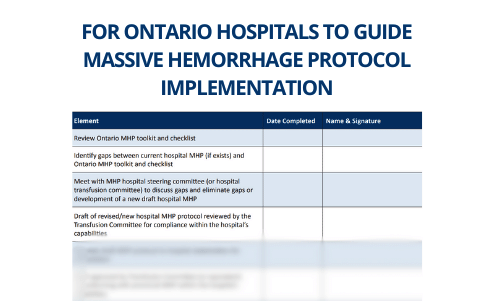
Implementation Checklist (MHP Toolkit) – Adult
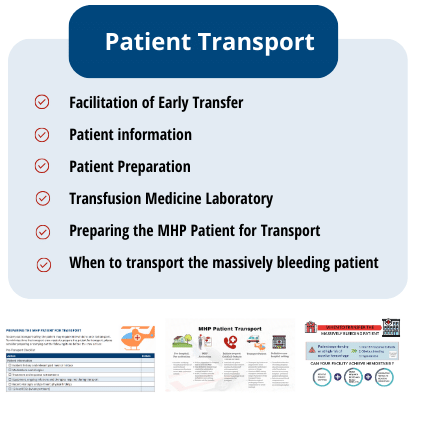
Patient Transport (MHP Toolkit)
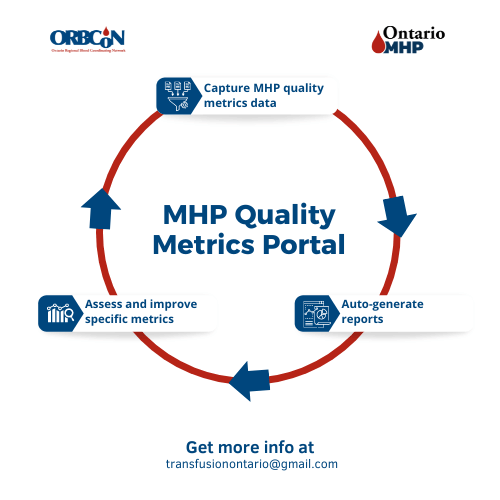
MHP Quality Metrics Portal
Note: Each Ontario hospital will need to determine where the data for the metrics is housed within their facility and who will be responsible for gathering and entering the data.
Upcoming Events
Transfusionists Talk
CSTM 2024

U of T

June 20, 2024 @12pm-1pm
MLT Session – Interesting serology cases
Subscribe to U of T Transfusion Medicine Rounds mailing list to get registration details