Small-Volume Tubes to Reduce Anemia and Transfusion (STRATUS) Clinical Trial
Dr. Deborah Siegal, MD MSc FCRPC, Hematologist (Thrombosis), The Ottawa Hospital
Associate Professor, Department of Medicine, University of Ottawa
Scientist, Clinical Epidemiology Program, Ottawa Hospital Research Institute
Patients with critical illness in the intensive care unit (ICU) are at high risk for anemia which affects 90% after only 3 days in ICU. About 40% of ICU patients receive at least one red blood cell (RBC) transfusion to correct anemia, half of which are given in the absence of active bleeding. Both anemia and RBC transfusion are associated with adverse outcomes including higher mortality, and longer ICU and hospital admission.
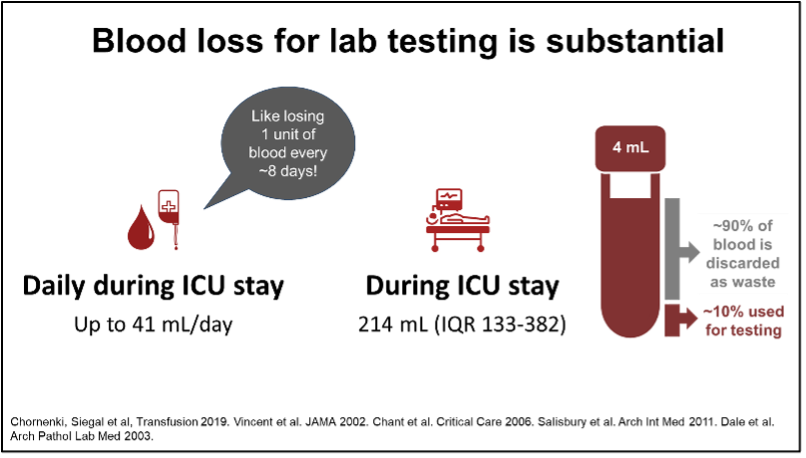
Although anemia is multifactorial, blood sampling for laboratory testing is substantial with volumes of 41 mL/day or more than 200 mL during ICU admission. This is like donating a unit of blood after 8 days in ICU. For each additional 150 mL drawn, the risk of RBC transfusion is increased 2-fold.
However, unlike healthy blood donors, ICU patients are unable to increase the production of RBCs to compensate for blood loss. Reducing RBC transfusion, a scarce and costly treatment with well-described risks, is viewed widely as a clinical priority for ICU patients.
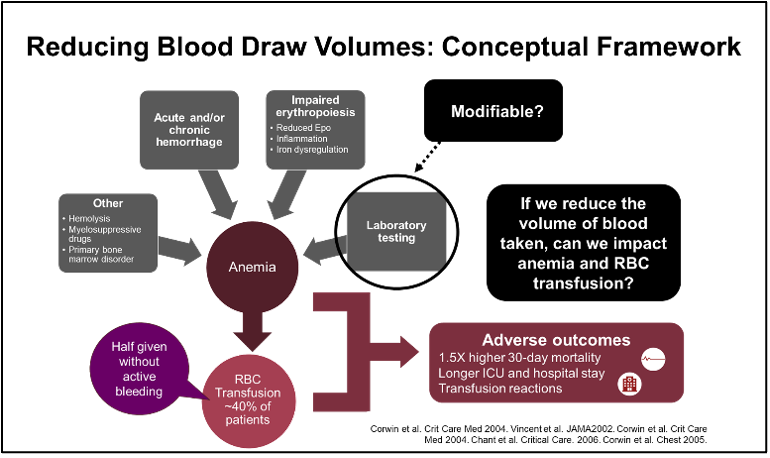
Laboratory testing, a modifiable contributor to anemia and RBC transfusion, is an ideal target because only 10% of the blood collected is required for testing and the remainder is discarded. However, there have been legitimate concerns about negative effects on laboratory testing, especially specimen sufficiency.
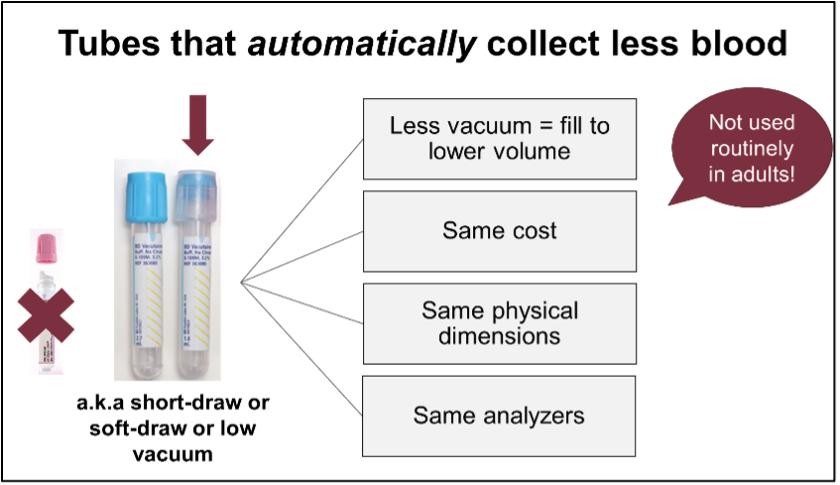
We conducted the Small-Volume Tubes to Reduce Anemia and Transfusion (STRATUS) Trial to test the hypothesis that switching to tubes that “automatically” collect less blood for lab testing (so called small-volume or low-vacuum tubes) reduces RBC transfusion in ICU patients (https://jamanetwork.com/journals/jama/fullarticle/2810758). These tubes have the same cost and size as the standard-volume tubes so are compatible with lab equipment, but they have lower vacuum and fill to a lower predetermined volume.
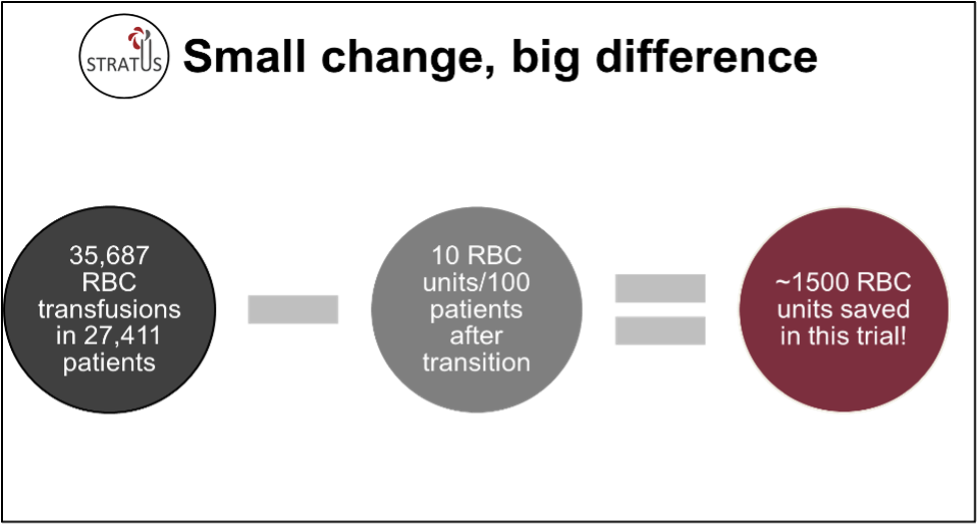
We used an innovative stepped wedge cluster randomized trial design in which ICUs switched from standard- to small-volume tubes according to a randomized schedule. STRATUS involved 25 academic and community ICUs in Canada with data collected from over 27,000 patients admitted to ICU for 48 hours or longer. Implementation of small-volume tubes reduced RBC transfusion during ICU admission by about 10 units per 100 patients. After switching to small-volume tubes, the decrease in hemoglobin during ICU admission was lower. Importantly, there was no negative effect on blood sample sufficiency. Although the COVID-19 pandemic affected study conduct and analyses, taken together, the findings support implementation of small-volume tubes.
Small-volume tubes were ordered using existing hospital infrastructure and implemented by hospital staff with brief targeted education. An important limitation is that non-ICU hospitalized patients were not included. However, reducing blood loss is expected to have broad benefit, as excess volume does not add value to care and may be harmful. Implementation strategies may be different in other settings.
While transition to small-volume tubes had a small effect on individual patients, if implemented widely, they have potential for significant impact on health systems and the blood supply. In STRATUS, over 36,000 RBC transfusions were given in less than 2 years; use of small-volume tubes saved about 1500 units of blood. Efforts to sustain the supply of blood products are critical to ensure they are available when needed especially during ongoing shortages in Canada.
Featured Resources
MHP 2.0

Upcoming Events
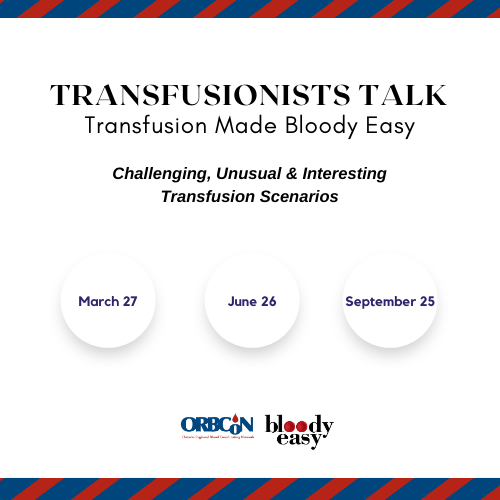
Transfusionists Talk
U of T Rounds

January 25, 2024 @12pm-1pm
Subscribe to U of T Transfusion Medicine Rounds mailing list to get registration details