Whither convalescent plasma therapy?
Dana V. Devine, PhD Chief Scientist, Canadian Blood Services and Director, UBC Centre for Blood Research
The concept of using the plasma from someone who has recovered from an illness to treat patients in the early stage of the same illness is not new. Our understanding of the immune system led to the development of this approach in the early 1900’s, and there was fairly widespread use of convalescent plasma to treat patients suffering in the 1918 influenza pandemic [1]. Seeking to determine whether this approach could be used as a therapeutic for treating patients with COVID-19, many clinical trials were set up around the world, including in Canada. The CONCOR-1 trial examined the effectiveness of COVID convalescent plasma (CCP) compared to routine patient care [2]. This trial was stopped early for futility as it became clear that the study would not achieve its statistical goal [3]. Similarly, the international REMAP CAP study which focused on ICU patients was also stopped for futility [4]. Studies that have shown success are characterized by very early use of CCP and use of a product that has a high titre of virus neutralizing antibodies [5]. This should not be surprising as we know that a typical person mounts an antibody response to a pathogen (or vaccine) within 5 days or so. The use of CCP may actually be detrimental to some patients as it creates a strong immune response that may actually worsen disease [3]. The US C3PO study also showed that treating patients with CCP pre-hospital but within 7 days of onset of symptoms did little to reduce disease progress [6].
Similarly, the preliminary clinical trials using hyperimmune immunoglobulins isolated from CCP have been similarly disappointing and most have been stopped at this point. Again, this probably has more do to with when the patient received the product.
Convalescent plasma may yet have a population of patients that it will help and those are patients who do not mount a robust antibody response because they are immunosuppressed either by underlying disease or immunosuppressive drugs taken by organ transplant recipients, for example. We should soon know if this is the target patient population for convalescent plasma therapy or if we need to develop strategies to identify patients much earlier in their disease course.
References:
1. Luke TC, Kilbane EM, Jackson JL et al. Meta-Analysis: Convalescent Blood Products for Spanish Influenza Pneumonia: A Future H5N1 Treatment? Ann. Intern. Med. 2006;145:599-609.
2. Bégin P, Callum J, Heddle NM, et al. Convalescent plasma for adults with acute COVID-19 respiratory illness (CONCOR-1): study protocol for an international, multicentre, randomized, open-label trial. Trials. 2021 May 4;22(1):323
3. Bégin P, Callum J, Jamula E, et al. Convalescent plasma for hospitalized patients with COVID-19: an open-label, randomized controlled trial. Nature Medicine 2021 Sep 9. doi: 10.1038/s41591-021-01488-2. Online ahead of print.
4. Estcourt LJ, Turgeon AF, McQuilten ZK et al. Effect of Convalescent Plasma on Organ Support-Free Days in Critically Ill Patients With COVID-19: A Randomized Clinical Trial. JAMA 2021 Oct 4;e2118178. doi: 10.1001/jama.2021.18178. Online ahead of print.
5. Libster R, Marc GP, Wappner D et al. Early High-Titer Plasma Therapy to Prevent Severe Covid-19 in Older Adults. N Engl J Med 2021 Feb 18;384(7):610-618
6. Korley FK, Durkalski-Mauldin V, Yeatts SD et al. Early Convalescent Plasma for High-Risk Outpatients with Covid-19. N Engl J Med 2021 DOI: 10.1056/NEJMoa2103784. On line ahead of print.
Patient Engagement in the CONCOR-1 Trial: Formation and Involvement of the Community Advisory Committee
Emily Sirotich BSc, PhD candidate, McMaster Centre for Transfusion Research.
Patient and public engagement in research is a growing movement to involve diverse stakeholders who bring relevant knowledge and experience to a research team. Partnerships between stakeholders are strengthened by joint development of the research design, implementation, analysis, and dissemination of results. Studies that engage stakeholders will improve generalizability, increase uptake of research findings, and integrate knowledge translation strategies; resulting in high quality research, informed by stakeholders that is more likely to be embraced by the community.
During the initial stages of the CONvalescent Plasma for Hospitalized Adults With COVID-19 Respiratory Illness (CONCOR-1) trial design, the Steering Committee recommended collaboration with community members to ensure the inclusion of diverse perspectives and lived experiences throughout the trial. It was especially important to engage with members from marginalized groups or populations who are underrepresented in research, as well as those most affected by COVID-19, to help advocate for their access to recruitment and results of the trial. The Community Advisory Committee (CAC) of the CONCOR-1 trial was formed prior to recruitment to engage with key stakeholders throughout the trial.
Trial investigators and CAC members collaborated to identify aspects of the clinical trial where community input would be beneficial. These areas included the: CONCOR-1 website, patient recruitment information and strategies, the patient consent process, plasma collection and distribution, challenges at the hospital level, public communication and knowledge translation strategies, as well as the final analyses. Throughout the CONCOR-1 trial, CAC members attended virtual, monthly meetings where study updates were provided, and CAC member input was sought into various aspects of the trial. Investigators recognized the importance of incorporating diverse perspectives and provided CAC members with the knowledge needed to understand the trial through educational sessions about COVID-19 antibodies, data safety monitoring and how to interpret study results.
The many available resources on patient and public engagement can help guide the process. However, the method of applying patient and public engagement strategies is unique to each research team and study. My experience joining the CAC team within the CONCOR-1 trial exemplified the benefits and importance of engaging with community members with diverse perspectives and lived experiences, especially through formal clinical trial study advisory groups. This learning experience highlighted that research will continue to improve when we invite more voices to the table.
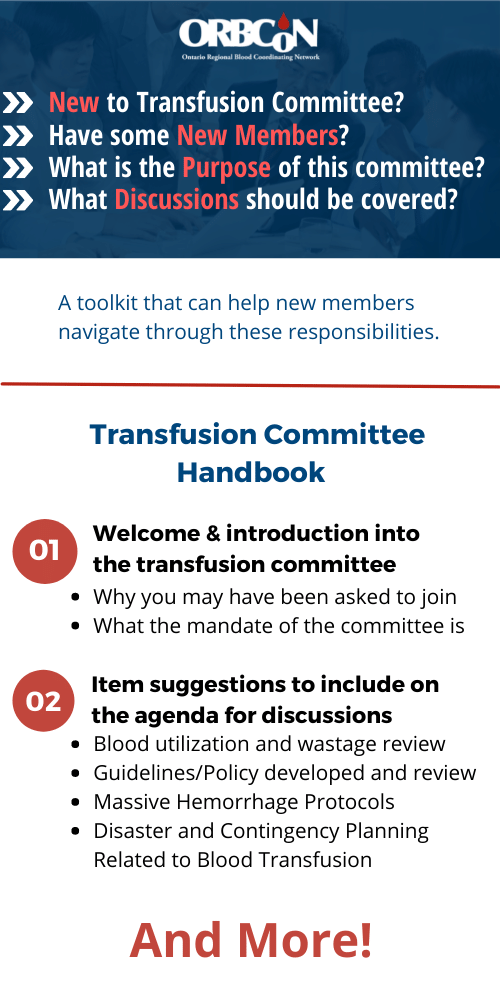
Featured Resource: Transfusion Handbook Committee

University of Toronto Transfusion Medicine Rounds
December 16th, 2021 @ 12:00 pm – 1:00 pm
MLT Session: Challenging Serology Cases, presented by Ms. Minda Agpalo, Dr. Waseem Anani, Dr. Celina Montemayor
