An Ethics Review of the Ontario Contingency Plan for the Management of Blood Shortages
Wendy Owens, Rebecca Barty, Troy Thompson Ontario Regional Blood Coordinating Network (ORBCoN)
Following a debrief of a blood shortage simulation exercise in Ontario held in 2018 (1), a recommendation was made that there should be a review done of the provincial blood shortage plan to ensure it meets ethical guidelines. In 2021, ORBCoN contacted an ethicist to request such a review be initiated. This article highlights the purpose of an ethical review and the recommendations put forth by the ethicist after a review of the provincial blood shortage plan was completed.
What is an ethical review?
An ethical review of a document or process is done to ensure if meets ethical standards meaning that decisions will be made based on certain values and principles. A good decision-making process helps to build trust, to increase legitimacy and acceptability of decisions, and to effectively implement them. Its hallmarks are:
Accountability: decision makers are answerable to the public for the type and quality of decisions made or actions taken.
Openness and transparency: decisions are made in such a way that stakeholders know, in a full, accurate and timely manner, what decisions are being made, for which reasons, and what criteria were applied, and have the opportunity to provide input.
Inclusiveness: groups and individuals who are most likely to be affected by a decision are engaged in the decision-making and planning processes to the greatest extent possible.
Responsiveness: decisions are revisited and revised as new information emerges.
Intersectionality: an intersectional lens is applied to deliberation and decision making. (2)
When decisions need to be made in healthcare under circumstances where resources are in short supply, basing decisions within an ethical framework can help ensure care will be provided in an equitable manner that can be understood and accepted by all those affected.
The review of the plan included seeking feedback from stakeholders in healthcare that would need to apply the plan if a blood shortage occurs (clinical decision makers) or those that might be affected by the decisions made as potential recipients of blood products during a supply shortage event.
Strengths of the Ontario Plan included the fact that is harmonized with the National Plan for the Management of Shortages of Labile Blood Components, (3) and the fact that it defines a clear and consistent staged process of steps to follow dependent on the severity of the shortage. Another strength identified was that step wise mitigation steps are listed to help avoid an actual shortage occurring and having to make decisions to restrict access to blood.
In addition to these strengths, the plan was complemented on the focus of preparedness and the simulation exercises that have been held to ‘test’ it out and to raise awareness amongst stakeholders. It was suggested that the participants in any future simulation exercises should be expanded to include more clinical decision-makers as well as representation from recipient groups, especially those that are from vulnerable populations. Through the review process it was clear that prescribers and clinically decision-makers have confidence and trust in the blood system which will be an advantage should supply constraints occur and allocation decisions need to be made.
The review included some recommendations for improving the Ontario Plan. These included:
- Improving inclusiveness and ensuring groups that have been marginalized in the past and excluded from decision making be consulted on any future iterations of the plan and be included in future simulation exercises. It was further suggested that adding training tools to help address awareness around these issues could improve the management of blood shortages within the province.
- Improving transparency through making the plan more available publicly to aid in awareness of how hard decisions may need to be made and that they will be based on ethical principles. One of these principles is to ensure a patient, even if they are assessed to not receive the resource that is in short supply, will not be abandoned and will continue to receive every other alternative treatment available.
- More preparation of clinical staff and hospital management will help ensure the decisions made in a blood shortage will be fair and just. Training of clinicians in their residency stage of education as well as development of tools and educational modules to support decision making would add value to the plan.
“The truth is, there will never be an easy or even distinctly ‘right way’ to make these decisions. Uncertainties will remain no matter what guidance is in place. However, some planning, support and other interventions can help mitigate primarily the moral harms faced by patients and secondly the effects of these hard decisions on decision-makers.” (4)
References:
- Ontario 2018 Blood Shortage Exercise Report https://transfusionontario.org/wp-content/uploads/2020/06/Ontario-2018-Blood-Shortage-Exercise-Report_Accessible.pdf
- https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/canadas-reponse/ethics-framework-guide-use-response-covid-19-pandemic.html
- National Plan for the Management of Shortages of Labile Blood Components Jan 2022. https://www.nacblood.ca/resources/shortages-plan/index.html
- Ethics review for the Ontario Contingency Plan for Management of Blood Shortages. Schwartz L; Dec 2021.
Competition
Register: Transfusion Medicine Technical Dry Workshop

Register: CSTM 2022 Annual Conference

Save the Date: Perinatal Consensus Conference
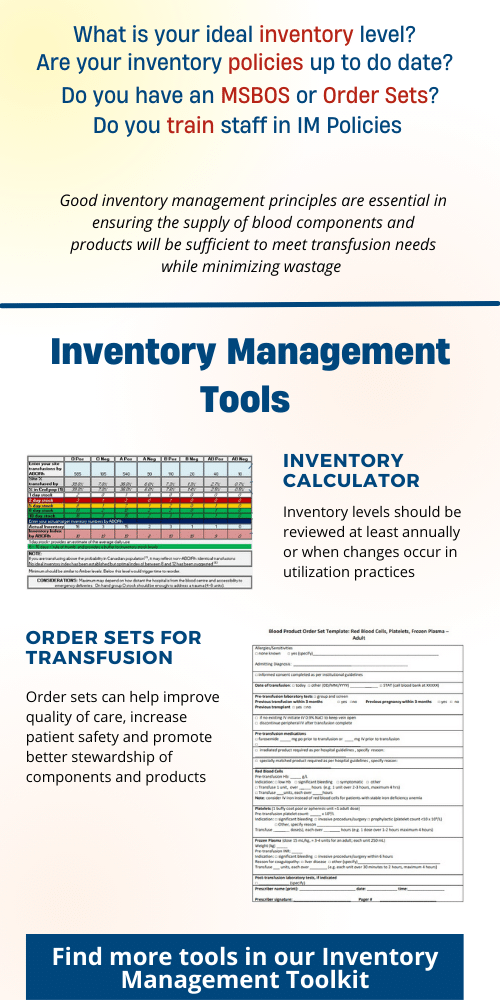
Featured Resource: Inventory Management Toolkit
Upcoming Event: University of Toronto Transfusion Medicine Rounds

March 24th, 2022 @ 12:00 pm – 1:00 pm
RhIG administration in early Pregnancy Now and Moving Forward presented by Dr. Dustin Costescu