CSTM Standards Version 5: What to expect in this version
Danielle Watson-Kinney CSTM Standards Committee (Chair),
Dr. Elaine Leung Haematopathologist; Division of Haematology and Transfusion Medicine Children’s Hospital of Eastern Ontario (CHEO)
The CSTM Standards for Hospital Transfusion Services, Version 5 were released December 2021, and reflects evidence based best practice in Canada. This bilingual document is compliant with the CAN/CSA-Z902-20, National Standard of Canada Blood and blood components and the Health Canada Blood Regulations. This user-friendly document is meant to support safe transfusion practice in hospitals and assist in meeting accreditation requirements in some jurisdictions.
A great deal of gratitude is to be given to the CSTM standards committee members for providing their expertise and sacrifice of their personal time in providing these standards. The CSTM standards committee is a group of 10 volunteers from regional, community, and rural transfusion services and from both pediatric and adult academic centers across Canada. The committee is a diverse group of professionals consisting of Medical Laboratory Technologists, Registered Nurses, Physicians, and one Quality Systems specialist.
Work on the current version started in January 2020 with all meetings held virtually. Under normal circumstances our team would meet in person at the annual CSTM conference to develop a working plan that aligns with Health Canada Regulations and CSA Z902-20 revisions, but unfortunately the pandemic prevented these face-to-face meetings. As this is a volunteer committee, we were at times challenged with coordinating meetings as members have full time jobs and family commitments.
There were numerous minor changes and updates made to Version 5, many of which were intended to clarify the existing standard. There were also some significant changes which include:
- the application of the requirement for confirmatory ABO testing of all recipients prior to transfusion of non-group O red cell units to all crossmatches, not just computer crossmatches
- addition of separate sections and expansion of the clauses related to the Health Canada requirements for errors and accidents and adverse transfusion reactions
- addition of a “general” section with respect to modification of blood components and blood products to provide guidance with respect to Health Canada expectations
- inclusion of x-ray irradiators
- recommendation for people 45 years or younger of childbearing potential to be transfused with K negative red cell units
- addition of the requirement for temperature monitoring of blood component and blood product shipments
- recommending that a policy for return of blood components and blood products to the Transfusion Service to include consideration for infection control
Guidance Statement Additions
- 3.1.2 Equipment
- 5.4.3.1 Selection for Transfusion of ABO Compatible Plasma
- 5.3.7.1.2 (formerly 5.3.7.3.3 Serological Testing Positive Patient Identification PPID)
The CSTM Standards for Hospital Transfusion Services are not meant to serve as an operating procedure manual but to provide standards for the development of policies, processes and procedures, which should be included in the institution’s policy and procedure manual. The CSTM guidance statements are developed for our hospitals nationally and come from your “Ask the Standards” questions and comments to our committee. Please continue to submit your questions and feedback so we can continue to thrive and make Canadian healthcare a place where quality and best practice comes first in all our transfusion facilities.
Lastly, ORBCoN will be purchasing the CSTM Standards version 5, 2021 for all hospitals in Ontario. CSTM Standards are protected under copyright laws and are not to be copied or redistributed. Your CSTM individual memberships provides you with access to the online copy. CSTM is a non-profit society, and you are encouraged to become involved in CSTM. Go to the website www.transfusion.ca for details on how to become an individual or institutional member. Please consider serving as a volunteer on one of the many committees – it’s a great way to meet others in the Canadian transfusion community. Without volunteers we wouldn’t be where we are today!
New! T-Shirt Design Competition
Register: Transfusion Medicine Technical Dry Workshop

Register: CSTM 2022 Annual Conference

Save the Date: Perinatal Consensus Conference
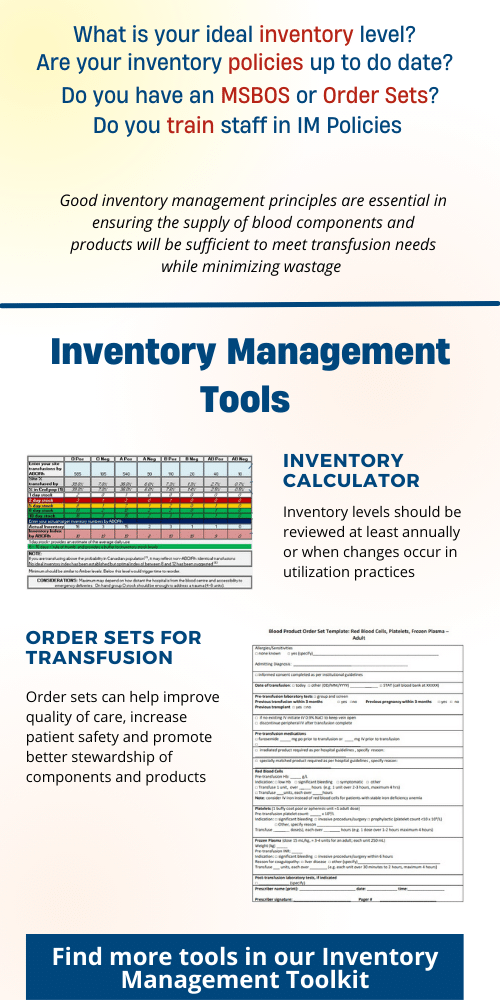
Featured Resource: Inventory Management Toolkit
Upcoming Event: University of Toronto Transfusion Medicine Rounds

March 24th, 2022 @ 12:00 pm – 1:00 pm
RhIG administration in early Pregnancy Now and Moving Forward presented by Dr. Dustin Costescu