January 2024

In This Issue
- Bloody Easy Blood Administration eLearning course- 2 Year Anniversary!
- MHP 2.0 – An Educational Symposium
- Small-Volume Tubes to Reduce Anemia and Transfusion (STRATUS) Clinical Trial
- Featured Resources
- MHP 2.0 Archive
- Upcoming Events
- Transfusionists Talk (Save the Dates)
- U of T Rounds
Bloody Easy Blood Administration eLearning course- 2 Year Anniversary!
Transfusionist Education and Competency Assessment: Bloody Easy
Troy Thompson- ORBCoN Program Manager and Donna Berta- ORBCoN Clinical Project Coordinator
The Canadian Transfusion Medicine standards mandate that all individuals performing activities related to blood transfusion participate in training and competency assessment programs1,2. The skills, theoretical and practical knowledge, essential to their role responsibilities must be addressed1,2. The Ontario Regional Blood Coordinating Network’s (ORBCoN) mission is “inspiring and facilitating best transfusion practices in Ontario”3.
The Bloody Easy Blood Administration eLearning course was re-developed/launched in December 2021. The course was developed to help hospitals with standards and accreditation requirements. Revisions to the BEBA eLearning module (figure 1) were based on principles of adult learning, recognizing transfusionists as mature learners with an abundance of prior learning experiences4,5. Module content is organized to align with the procedural steps for blood administration. Interactive activities are a strategic design element to inform learning (figure 2). The assessment quiz incorporates scenario-based questions and provides immediate explanation for the correct responses. For successful completion, 80 percent correct responses are required (multiple attempts are permitted). Expertise in clinical content and innovative use of software simulation tools supported the module development process. The material is reinforced by the BEBA handbook, a widely used clinical practice reference.
The BEBA eLearning module is available to Ontario facilities via ORBCoN’s Sharable Content Object Reference Model (SCORM) files and through a Canadian health care focused Learning Management System (LMS) provider. The LMS provider enables ORBCoN to independently track eLearning utilization, specifically aggregate assessment quiz responses. These outcome metrics will endorse ongoing appraisal of the module and identification of knowledge gaps to be addressed.
Since December 2021, the inaugural year, there has been significant uptake of the eLearning course. Approximately 41 facilities accessed the SCORM files for their site. Data from the LMS provider reported an additional 129 facilities (including 12 colleges/universities) and over 7500 individuals have utilized the module (figure 3).


List of hospitals (with permission) per “Pre-hospital site visit” survey results (as of Dec 7, 2023); not all hospitals participated in this survey.
The BEBA eLearning module was updated to reflect self-directed learning, current TM standards and best practices. There has been positive uptake of the module by hospitals as well as colleges and universities. Quiz outcome metrics will be analyzed to identify foci for further learning. The BEBA eLearning module serves to meets the mandate of the Canadian standards, while also informing clinical practice to enhance the safety of blood transfusion. The current eLearning module and quiz will be further revised in 2024/25.
REFERENCES
- National Standard of Canada Canadian Standards Association (CA) Blood and blood components. Toronto ON; 2020 Mar 24; cited 2023 Mar 10. 162 p. Report No.: CAN/CSA-902:20. Available from: https://community.csagroup.org/docs/DOC-126295
- Canadian Society for Transfusion Medicine (CA) Standards for hospital transfusion services. Markham ON; 2021 Dec 1 [revised 2022 Dec cited 2023 Mar 10]. 114 p. Report No.: Version 5. Available from: https://www.transfusion.ca/Resources/Standards
- Ontario Regional Blood Coordinating Network. About us [Internet]. [Place unknown]: Ontario Regional Blood Coordinating Network; 2006 [revised 2020 cited 2023 Mar 10]. Available from: https://transfusionontario.org/en/about/
- Knowles MS. The modern practice of adult education: from pedagogy to andragogy. Rev. and updated. Wilton, Connecticut. Chicago: Association Press; 1980. 400 p.
- Hutchinson AM, Estabrooks CA. Educational theories. In: Straus SE, Tetroe J, Graham ID, editors. Knowledge translation in health care: moving from evidence to practice. 2nd ed. Hoboken, New Jersey: Wiley Blackwell BMJ Books; 2013. p. 298-307.
MHP 2.0 – An Educational Symposium
ORBCoN, Central Region
On November 9th 2023, 109 multi-disciplinary healthcare professionals from across Ontario and beyond attended ORBCoN’s Massive Hemorrhage Protocol (MHP) 2.0 educational symposium. The goal of the symposium was to bring together stakeholders to present new topics relevant to the massively bleeding patient, provoke discussion and share the latest in evidence that may impact the current iteration of Ontario’s First Recommendations of Massive Hemorrhage Protocol.
The educational event focused on the following 3 fundamental questions:
1. What have we learned?
- data on provincial survey results and pilot data on quality metrics portal
2. What can we expect?
- Impending changes due to new products, new trials and new publications
3. What do we do next to update recommendations and improve current practice?
- pre-hospital red blood cell transfusion; Tranexamic acid
- clinical event debrief
- addressing barriers to change
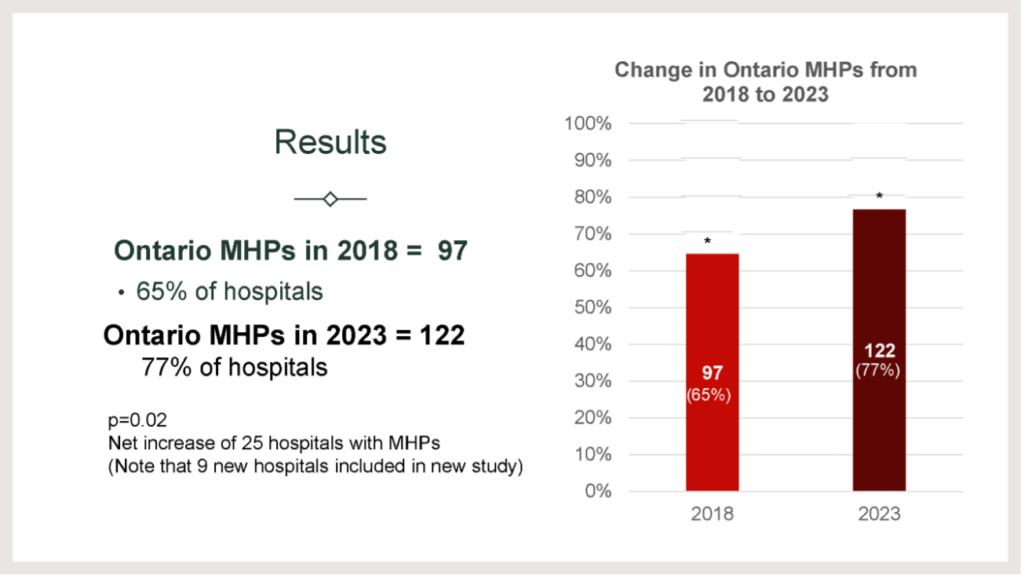
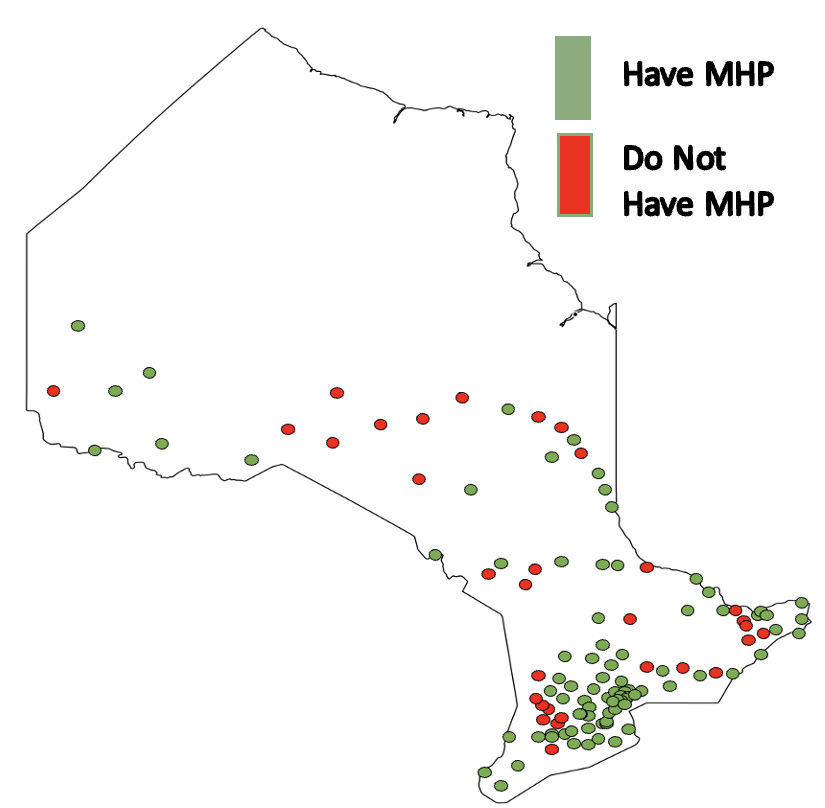
As illustrated in figure 1 below, a significant improvement in the number of hospitals with a formal MHP in place with a net increase of 25 hospitals since 2018.
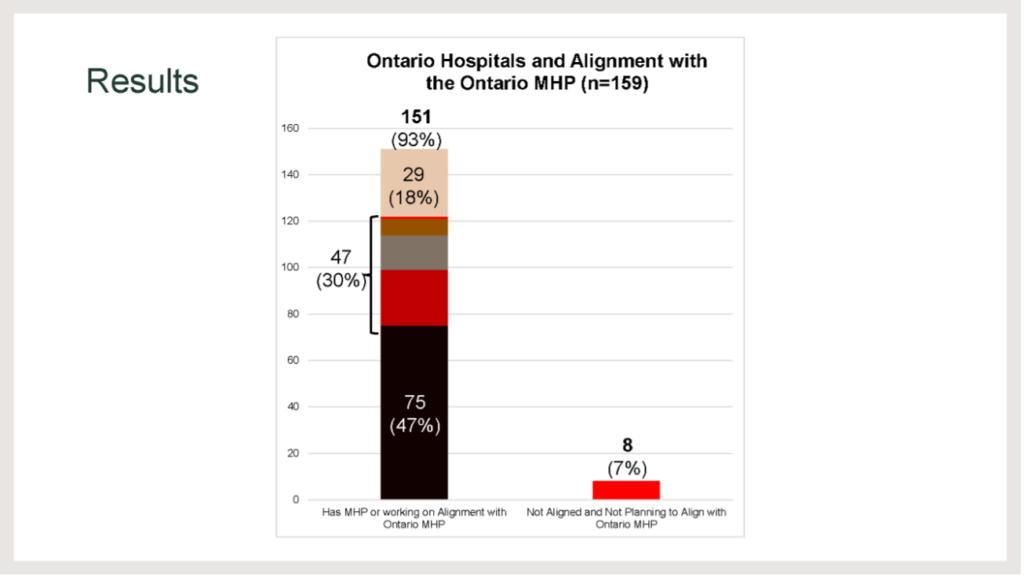
47% (75) of hospitals have a formal MHP in place. A further 30% (47) indicated they were partially aligned with the Ontario Recommendations. 37% do not have an MHP in place however, 18% (29) of those who do not indicated that they were currently working towards a protocol and alignment with Ontario Recommendations. 7% (8) of hospitals (7 small and 1 large) in Ontario do not have an MHP in place and are not currently working towards one at the time of survey.

We hear you!! … but patients with massive hemorrhage can present to any hospital.
- Ensure you have a policy to transfer the patient out for definitive damage control.
- Leverage the resources you have. Consider a regional policy or learn how others with similar size and services manage or check out the non-definitive setting checklist available to you.
Although huge strives have been made in the province over the last five years to standardize the care of the massively bleeding patient, there remains room for improvement. As we work on MHP 2.0 in 2024 we will look to continue to reduce policy variability, increase inclusion of pediatric provisions for those hospitals that care for children (only 56 hospitals out of 101 who indicated they care for patients under the age of 18 include provisions for population) and continue to ensure quality assurance and adherence.
Presentations have been archived and can be found here
Small-Volume Tubes to Reduce Anemia and Transfusion (STRATUS) Clinical Trial
Dr. Deborah Siegal, MD MSc FCRPC, Hematologist (Thrombosis), The Ottawa Hospital
Associate Professor, Department of Medicine, University of Ottawa
Scientist, Clinical Epidemiology Program, Ottawa Hospital Research Institute
Patients with critical illness in the intensive care unit (ICU) are at high risk for anemia which affects 90% after only 3 days in ICU. About 40% of ICU patients receive at least one red blood cell (RBC) transfusion to correct anemia, half of which are given in the absence of active bleeding. Both anemia and RBC transfusion are associated with adverse outcomes including higher mortality, and longer ICU and hospital admission.
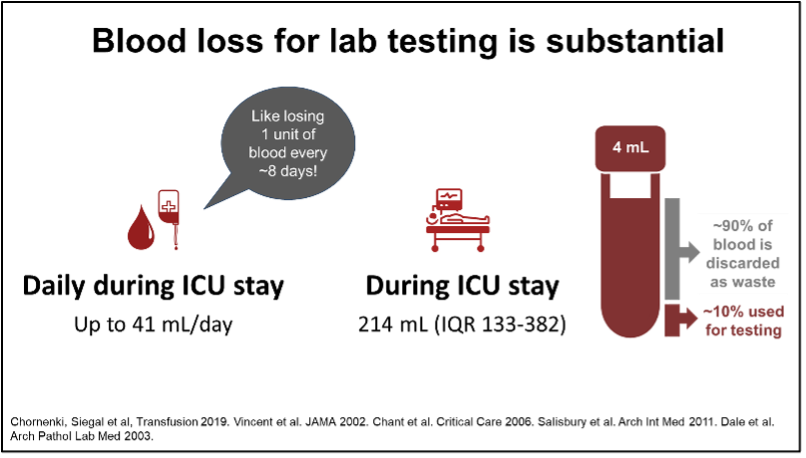
Although anemia is multifactorial, blood sampling for laboratory testing is substantial with volumes of 41 mL/day or more than 200 mL during ICU admission. This is like donating a unit of blood after 8 days in ICU. For each additional 150 mL drawn, the risk of RBC transfusion is increased 2-fold.
However, unlike healthy blood donors, ICU patients are unable to increase the production of RBCs to compensate for blood loss. Reducing RBC transfusion, a scarce and costly treatment with well-described risks, is viewed widely as a clinical priority for ICU patients.
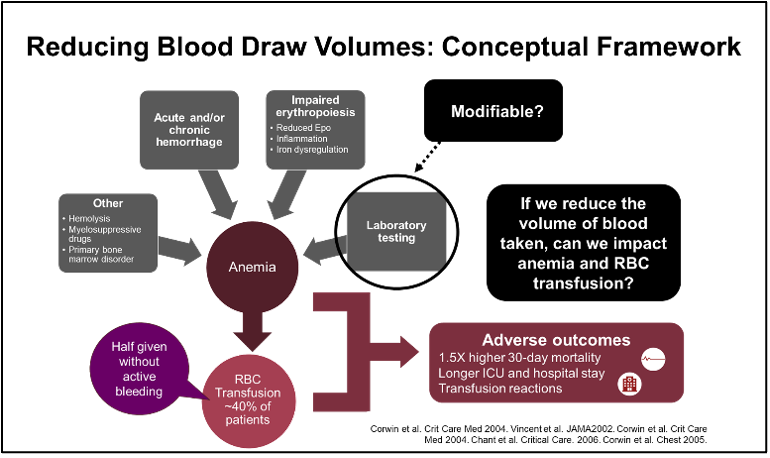
Laboratory testing, a modifiable contributor to anemia and RBC transfusion, is an ideal target because only 10% of the blood collected is required for testing and the remainder is discarded. However, there have been legitimate concerns about negative effects on laboratory testing, especially specimen sufficiency.
We conducted the Small-Volume Tubes to Reduce Anemia and Transfusion (STRATUS) Trial to test the hypothesis that switching to tubes that “automatically” collect less blood for lab testing (so called small-volume or low-vacuum tubes) reduces RBC transfusion in ICU patients (https://jamanetwork.com/journals/jama/fullarticle/2810758). These tubes have the same cost and size as the standard-volume tubes so are compatible with lab equipment, but they have lower vacuum and fill to a lower predetermined volume.
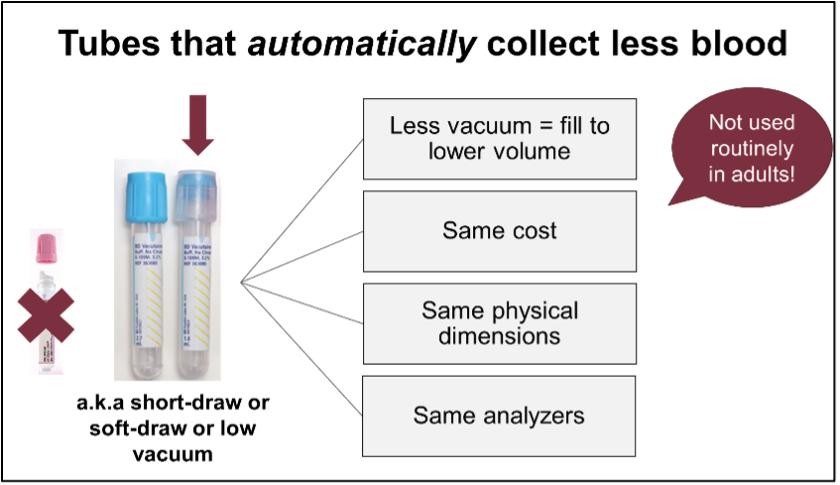
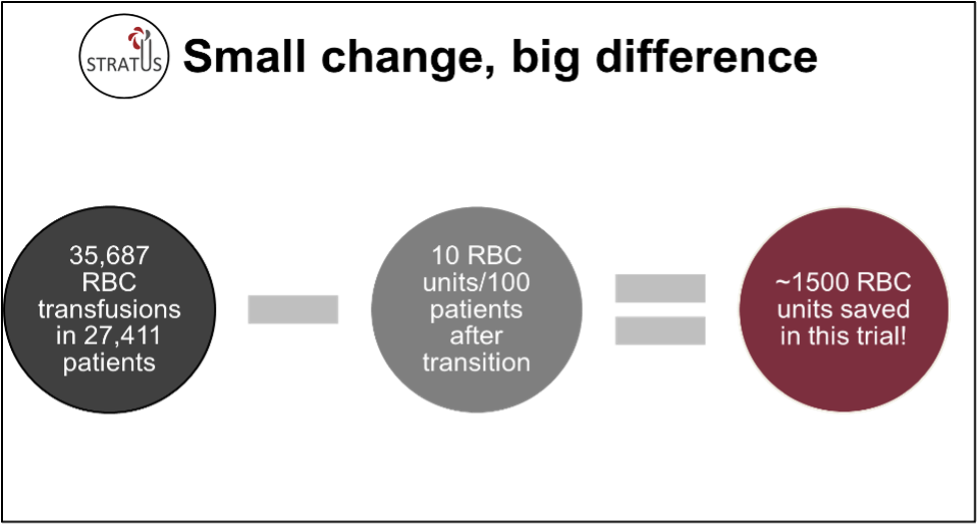
We used an innovative stepped wedge cluster randomized trial design in which ICUs switched from standard- to small-volume tubes according to a randomized schedule. STRATUS involved 25 academic and community ICUs in Canada with data collected from over 27,000 patients admitted to ICU for 48 hours or longer. Implementation of small-volume tubes reduced RBC transfusion during ICU admission by about 10 units per 100 patients. After switching to small-volume tubes, the decrease in hemoglobin during ICU admission was lower. Importantly, there was no negative effect on blood sample sufficiency. Although the COVID-19 pandemic affected study conduct and analyses, taken together, the findings support implementation of small-volume tubes.
Small-volume tubes were ordered using existing hospital infrastructure and implemented by hospital staff with brief targeted education. An important limitation is that non-ICU hospitalized patients were not included. However, reducing blood loss is expected to have broad benefit, as excess volume does not add value to care and may be harmful. Implementation strategies may be different in other settings.
While transition to small-volume tubes had a small effect on individual patients, if implemented widely, they have potential for significant impact on health systems and the blood supply. In STRATUS, over 36,000 RBC transfusions were given in less than 2 years; use of small-volume tubes saved about 1500 units of blood. Efforts to sustain the supply of blood products are critical to ensure they are available when needed especially during ongoing shortages in Canada.
Featured Resources
MHP 2.0

Upcoming Events
Transfusionists Talk
U of T Rounds

January 25, 2024 @12pm-1pm
Subscribe to U of T Transfusion Medicine Rounds mailing list to get registration details