Lessons Learned from a Multi-Code Event
Deborah Flowers, MLT, Charge Technologist Transfusion Medicine, EORLA
Most medical laboratory professionals are accustomed to the constant codes that sound overhead. On October 27, 2023, the Ottawa Hospital General Campus called an unprecedented Code Red, Code Orange and Code Grey, all within a few hours. Our team worked extremely well together under stress and solved emerging problems quickly, but could things have gone better? More importantly, what did we learn from our missteps?
Shortly before 4 pm, a Code Red was announced, and we were on emergency power. Not a cause for concern since critical areas like Transfusion Medicine are equipped with UPSs and an abundance of emergency plugs. Moments later, the lights flickered oddly, and a strange smell overtook the laboratory. In the days preceding, we had experienced several codes however this was different; it felt different. Someone suggested we prepare for evacuation, so we packed products into our Code Orange boxes and transferred the calls to the portable phone. When the notice came, we were ready. We grabbed our blood boxes, walked down the stairs, and set up in the Emergency Department garage. It wasn’t ideal but we were functional. We took inventory of the items we were missing, a charger for the portable phone, our external phone list, a pen. Small items that would have made our situation easier. Our first product request was for platelets which we hadn’t even thought to bring with us.
The Code Orange was next. Many of us have been involved in External Code Orange scenarios however never an internal disaster. It was surreal to see the Emergency Department deserted except for Emergency Response Personnel. Ambulances were diverted, patients were evacuated, transferred and discharged. We had already initiated our Code Orange policy, making it work for an internal disaster, so we continued.
Then a Code Grey was called, and we learned that emergency power had been lost to some parts of the hospital. No one could have imagined we would need a back-up for the back-up system. The next day when it was safe to return to the laboratory, it was an eerie scene. The smell was overpowering, and soot covered everything. The disaster cleanup would eventually take months to complete but we were back in Transfusion Medicine 24 hours after the first alarm sounded.
I don’t suggest laboratories plan to relocate as we did. In our situation, it was safe to bring blood products with us; we had time before the evacuation came. What was the most important lesson we learned? Effective communication is crucial in an infrastructure failure. In the beginning, our information was collected around a dying cell phone listening to situational updates. My advice to all medical laboratory professionals – review your contingency plan and recognize that communication is crucial. As Arthur Conan Doyle said, “It is easy to be wise after the event.”
Featured Resources
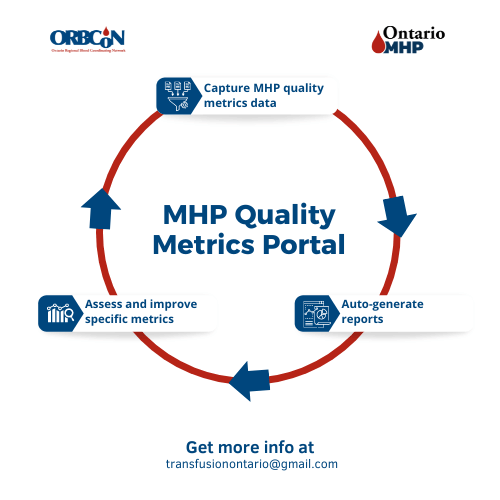
MHP Quality Metrics Portal
Note: Each Ontario hospital will need to determine where the data for the metrics is housed within their facility and who will be responsible for gathering and entering the data.
Upcoming Events
Transfusionists Talk
GHEST 2024 Save the Date

U of T

June 20, 2024 @12pm-1pm
MLT Session – Interesting serology cases
Subscribe to U of T Transfusion Medicine Rounds mailing list to get register