Are we over activating Massive Hemorrhage Protocols in Pediatric Patients?
Dylan Grimm1, Laurence Delorme1, Eric Fagan1, Na Li 2, Mark McVey3,4, Suzanne Beno5,6, Elaine Leung7,8, Lani Lieberman9,10, Troy Thompson11, Katerina Pavenski12, Jeannie Callum13, Kimmo Murto14,15
1Queen’s University, Faculty of Medicine, Kingston, ON; 2Centre for Health Informatics, University of Calgary, Calgary, AB; 3Hospital for Sick Children, Toronto, ON; 4Assistant Professor, University of Toronto, Department of Anesthesiology & Pain Medicine, Toronto, ON; 5Associate Professor, University of Toronto, Department of Pediatrics, Division of Emergency Medicine, Toronto, ON; 6Hospital for Sick Children, Toronto, ON; 7Assistant Professor, University of Ottawa Department of Pathology and Laboratory Medicine, Division of Hematology and Transfusion Medicine, Ottawa, ON; 8Children’s Hospital of Eastern Ontario (CHEO), Ottawa, ON; 9Assistant Professor, University of Toronto, Department of Laboratory Medicine & Pathology, Toronto, ON; 10University Health Network: Toronto General Hospital, Toronto, ON; 11Ontario Regional Blood Coordinating Network, Toronto, ON; 12Department of Laboratory Medicine and Pathobiology, University of Toronto, Toronto, ON; 13Professor, Department of Pathology and Molecular Medicine, Queen’s University, Kingston, ON; 14Associate Professor, University of Ottawa, Department of Anesthesiology & Pain Medicine, Ottawa, ON; 15CHEO Research Institute, Ottawa, ON.
Hemorrhage is the leading cause of preventable death within the first 24 hours after trauma in children and adults. In May 2021, the Ontario Regional Blood Coordinating Network (ORBCoN) disseminated the first provincial pediatric and adult evidence-based massive-hemorrhage-protocol (MHP) and associated toolkit content including recommendations for 8 quality improvement (QI) metrics.1,2 The initial QI data have provided insight on MHP trends in Ontario hospitals, and highlighted differences between adult and pediatric MHP activations.
MHP activation data and 28 day follow-up from 8 Ontario hospitals including 2 pediatric tertiary care centers was retrospectively collected (January 2019-May 2022). Patient demographics, mortality rates and 8 MHP QI metrics were entered in REDCap© data-collection-tool, and differences between adult versus pediatric MHP quality metrics were assessed.
In total, 363 MHP activations were reported and available for comparison (44 pediatric, 319 adult) (Table 1). Hemorrhage from traumatic injury accounted for most activations in children (59%) and adults (40%). Analysis of the QI metrics (Table 2) showed children were more likely to experience MHP over-activation (66 vs. 39%, p=0.002; correct activation defined as blood component requirements of adults>6 RBC units; children> 40 ml/kg, or death due to bleeding within first 24-hours) and less likely to experience a delay in RBC transfusion (4.5 vs 13%, p=0.003 (defined as > 15 minutes from protocol activation). Both cohorts reported ≥ 20% of patients had delayed tranexamic acid (TXA) administration and both cohorts had 11% of patients with uncorrected hypothermia at MHP termination. RBC over-transfusion (Hgb>110 g/L at MHP termination) was common and reported in 45% and 31% of children and adults, respectively, and 9.1% and 16% in children and adults reported blood component wastage.
MHP over-activation was more common in children compared with adults, with pediatric patients tending to see more unecessary activations as well as over-transfusions. One possible explanation is that hemorrhagic shock in pediatric patients may have a delayed onset or be more challenging to diagnose. However, these concerns should be balanced against transfusion risks, including hyperkalemia, hypoglycemia, and circulatory overload. In both cohorts, timely administration of TXA and management of hypothermia should be improved, as both have been shown to improve mortality in hemorrhage.
One limitation of this analysis is low numbers of pediatric MHP activations. However, at the time of this newsletter publication, there will be approximately 1700 MHP activations collected in the RedCAP® system, around 100 of which are expected to be pediatric activations. The data analysis is ongoing. The MHP QI metrics system is a valuable tool to identify the areas of improvement, with an overall goal of improving outcomes in patients receiving MHP.
Table 1. Demographics of pediatric and adult massive hemorrhage protocal activation cohorts
| Variable | Overall N=363 | Pediatric, N = 44 | Adult, N = 319 |
| MHP Activation Age, n (%) | |||
| Neonate (≤ | 3 (0.8) | 3 (6.8) | 0 (0) |
| Pediatric (>1 month to 12 yrs) | 22 (6.1) | 22 (50) | 0 (0) |
| Adolescent (13-17 yrs) | 19 (5.2) | 19 (43) | 0 (0) |
| Adult (>17 yrs) | 319 (88) | 0 (0) | 319 (100) |
| MHP activations by hospital, n (%) | |||
| B | 10 (2.8) | 0 (0) | 10 (3.1) |
| C | 33 (9.1) | 33 (75) | 0 (0) |
| D | 61 (17) | 2 (4.5) | 59 (18) |
| E | 87 (24) | 1 (2.3) | 86 (27) |
| F | 37 (10) | 1 (2.3) | 36 (11) |
| G | 3 (0.8) | 0 (0) | 3 (0.9) |
| H | 5 (1.4) | 5 (11) | 0 (0) |
| I | 127 (35) | 2 (4.5) | 125 (39) |
| MHP Activation Location, n (%) | |||
| ER | 209 (58) | 29 (66) | 180 (56) |
| OR | 46 (13) | 4 (9.1) | 42 (13) |
| Ward | 14 (3.9) | 0 (0) | 14 (4.4) |
| ICU | 80 (22) | 9 (20) | 71 (22) |
| Obstetrics | 10 (2.8) | 0 (0) | 10 (3.1) |
| Other | 4 (1.1) | 2 (4.5) | 2 (0.6) |
| MHP Type, n (%) | |||
| Trauma | 155 (43) | 26 (59) | 129 (40) |
| Gastrointestinal bleed | 88 (24) | 2 (4.5) | 86 (27) |
| Surgical bleed non-cardiac surgery | 29 (8.0) | 4 (9.1) | 25 (7.8) |
| Cardiac surgery | 13 (3.6) | 1 (2.3) | 12 (3.8) |
| Obstetrics | 18 (5.0) | 0 (0) | 18 (5.6) |
| Vascular | 25 (6.9) | 4 (9.1) | 21 (6.6) |
| Other | 32 (8.8) | 7 (16) | 25 (7.8) |
| Unknown | 3 (0.8) | 0 (0) | 3 (0.9) |
| Status at hospital Discharge up to 28 days, n (%) | |||
| Home | 154 (43) | 19 (43) | 135 (43) |
| Rehab | 29 (8.2) | 5 (11) | 24 (7.7) |
| Chronic Care | 21 (5.9) | 1 (2.3) | 20 (6.4) |
| Deceased | 151 (43) | 19 (43) | 132 (42) |
| N/A – Patient expired before 60 mins | 26 (7.2) | 0 (0) | 26 (8.2) |
| N/A – No transfer/definitive care provided | 254 (70) | 43 (98) | 211 (66) |
Table 2: Comparison of pediatric with adult massive hemorrhage protocol quality indicators, years 2019-2022
| Primary Outcomes, n (%) | Pediatric (N=44) | Adult (N=319) | p-value* |
| System-related: Proportion of MHP over-activation [adults>6 RBC units; children> 40 ml/kg or death due to bleeding within first 24-hours] | 29 (66) | 124 (39) | 0.002 |
| Process-related: Proportion of patients not administered RBCs within 15 mins of MHP activation | 2 (4.5) | 41 (13) | 0.003 |
| Proportion of patients not receiving TXA within 1 hour of MHP Activation | 12 (27) | 64 (20) | 0.322 |
| Patient-related: Proportion not achieving temperature ≥ 35°C at MHP termination | 5 (11) | 35 (11) | >0.99 |
| Secondary Outcomes, n (%) | |||
| System-related: Proportion where initiation for patient transfer did not occur within 60 minutes of MHP activation | 0 (0) | 27 (8.5) | <0.001 |
| Process-related: Proportion not transitioned to group-specific RBCs and plasma within 90 mins of arrival/onset of hemorrhage | 2 (4.5) | 21 (6.6) | 0.085 |
| Proportion of patients with blood component/product wastage | 4 (9.1) | 52(16) | 0.39 |
| Patient-related: Proportion with Hgb levels < 60 g/L | 0 (0) | 16 (5.0) | 0.35 |
| Proportion Hgb levels > 110 g/L | 20 (45) | 100 (31) | 0.14 |
Note: MHP=massive hemorrhage protocol; RBC=red blood cell; TXA=tranexamic acid; Hgb=hemoglobin
References:
- Callum JL, Yeh CH, Petrosoniak A, et al. A regional massive hemorrhage protocol developed through a modified Delphi technique. CMAJ. 2019;7(3):E546-E561.
- Cope S, Callum J, Pavenski K, et al. Ontario’s Massive Hemorrhage Toolkit. Transfus Med Rev. 2022;36(1):67.
- Holcomb JB, Moore EE, Sperry JL, et al. Evidence-Based and Clinically Relevant Outcomes for Hemorrhage Control Trauma Trials. Ann Surg. 2021;273(3):395-401.
- Leonard JC, Josephson CD, Luther JF, et al. Life-Threatening Bleeding in Children: A Prospective Observational Study. Crit Care Med. 2021;49(11):1943-1954.
Announcement
Tech Assessment
The Bloody Easy Technologist Assessment program is available on the new ORBCoN Learning Management System (LMS) and Surge Learning platforms.
A communication will be coming with instructions to provide site administrator information for access to the ORBCoN LMS and guidance for current Surge Learning clients.
If you have any questions please reach out to alison.wendt@sunnybrook.ca
Featured Resources
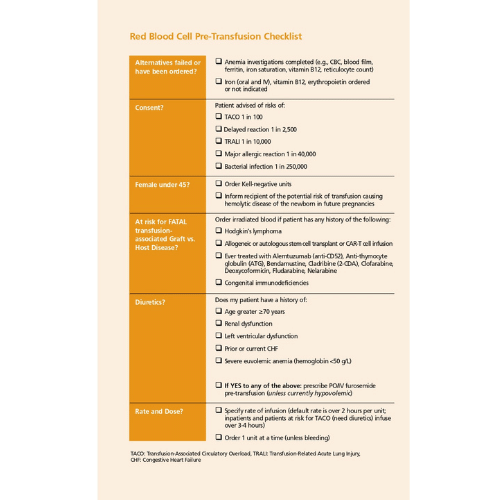
Bloody Easy 5: RBC Pre-Transfusion Checklist
Patient Pamphlet: New Version
Upcoming Events
UofT TM Rounds

December 15, 2022 @12pm-1pm
Running Big Data by Dr. Ruchika Goel
Virtual Session Only
Happy Holidays!
