May 2021


Massive Hemorrhage Protocol: Quality Metrics Reporting
Troy Thompson,
Regional Manager, ORBCoN CE Region
The use of quality metrics in healthcare is not a new concept. The reporting and analysis of quality metrics promotes improvement and increases transparency within the healthcare system. Standardized quality metrics have been developed for the Provincial Massive Hemorrhage Protocol (MHP) to help assess and improve specific activities over time at individual hospitals and will allow for peer benchmarking.
There are 8 quality metrics recommended for reporting in the MHP toolkit in order to assess the MHP process at your institution.
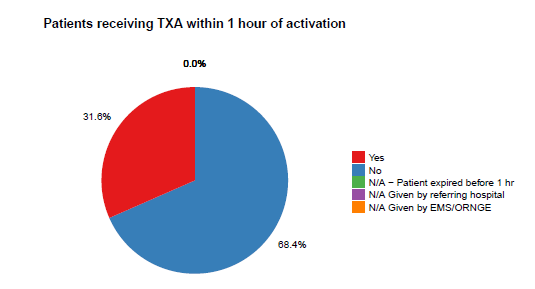
- The proportion of patients receiving tranexamic acid within 1 hour of protocol activation.
- The proportion of patients in whom RBC transfusion is initiated within 15 minutes of protocol activation.
- The proportion of patients (requiring transfer for definitive care) with initiation of call for transfer within 60 minutes of protocol activation.
- The proportion of patients achieving a temperature >35⁰C at termination of the protocol.
- The proportion of patients with hemoglobin levels maintained between 60-110 g/L during protocol activation, excluding certain pediatric populations (e.g. neonates) that may require higher hemoglobin values.
- The proportion of patients transitioned to group specific RBCs and plasma within 90 minutes of arrival/onset of hemorrhage.
- The proportion of patients with appropriate activation (>6 RBC units in first 24 hours; >40 ml/kg/24 hours of RBCs in pediatric patients) or before this level in patients dying due to hemorrhage within 24 hours.
- The proportion of patients without any blood component wastage (including plasma that is thawed and not used within the 5 day limit on another patient).
A Quality Metrics reporting portal has been developed to capture all of the 8 MHP quality metrics. The reporting portal is a validated and free tool that will allow users to report on and monitor their facility specific quality metrics. The portal will also be interfaced to a “dashboard” or data visualization tool which will provide a dynamic and interactive tool allowing users to quickly visualize and evaluate their metrics over time as well as against provincial benchmarks. Graphs as illustrated below will provide users with aggregate data for each quality metric entered by their site.
Site Specific Quality Metric Reporting
The use of a data visualization tool or “dashboard” for healthcare related activities provides hospital sites with a performance management tool that can measure, monitor and manage performance and quality improvement initiatives more effectively. These tools provide a dynamic platform for transmitting, analyzing and displaying metrics in “real time”. Access to “real time” data allows users to identify problem areas, root causes and make performance improvements quickly. The development, standardization and reporting of provincial MHP quality metrics will allow users to benchmark their own performance and provide provincial benchmarks for comparison. Detecting “outliers” or unacceptable performance will promote quality improvement initiatives ultimately leading to better patient care.
ORBCoN held an educational forum on April 30th to officially launch the provincial MHP Toolkit. Dr. Avery Nathens discussed in his presentation the importance of reviewing all activations for quality assurance purposes. He highlights strategies to implement and monitor the 8 quality MHP metrics and explains how we can learn and use the data from both the local and provincial metrics.
Dr. Nathen’s archived presentation along with the other presentations from the April 30th virtual event can be found here.
For more information regarding the Provincial Massive Hemorrhage Protocol (MHP) please visit https://transfusionontario.org/category/massive-hemorrhage-protocol/
References
Callum JL, Yeh CH, Petrosoniak A, et al. A regional massive hemorrhage protocol developed through a modified Delphi technique. CMAJO 2019 Sep 3;7(3):E546-E561.
May 27th: CBS Inventory and Engineering perspectives in Future presented by Mr. Rick Prinzen

Pairing Laboratory and Clinical Knowledge to Provide Better Care for Patients Who are Difficult Matches.
Tracy Cameron MLT 1, Wendy Owens ART 1, Waseem Anani MD2, Sheena Scheuermann MLT1, Allison Collins MD1, Julia Gilmore2, Irene Dines2, Hertha Hughes MLT3
Ontario Regional Blood Coordinating Network1, Canadian Blood Services2, Quinte HealthCare, Belleville General Hospital3
On April 13th and 14th, 2021, the Ontario Regional Blood Coordinating Network (ORBCON) partnered with Canadian Blood Services (CBS) to hold the 16th annual transfusion medicine educational event. This year, the event combined both practical and theory-based learning for health care professionals in Ontario. The theme of this event was ‘Game, Set and Match’ which focused on patients with a high incidence of alloimmunization.
Approximately one month before the event, blind samples were prepared and shipped to 50 hospitals across the province who had registered to participate. Samples and accompanying case scenarios were provided for three Tiers of testing:
- Tier 1 hospitals with minimal capability to perform transfusion related testing (ABO blood group and Rh type and antibody screen only)
- Tier 2 hospitals licensed to perform basic antibody identification and
- Tier 3 tertiary care sites with the capability of identifying rare and more complicated antibody cases
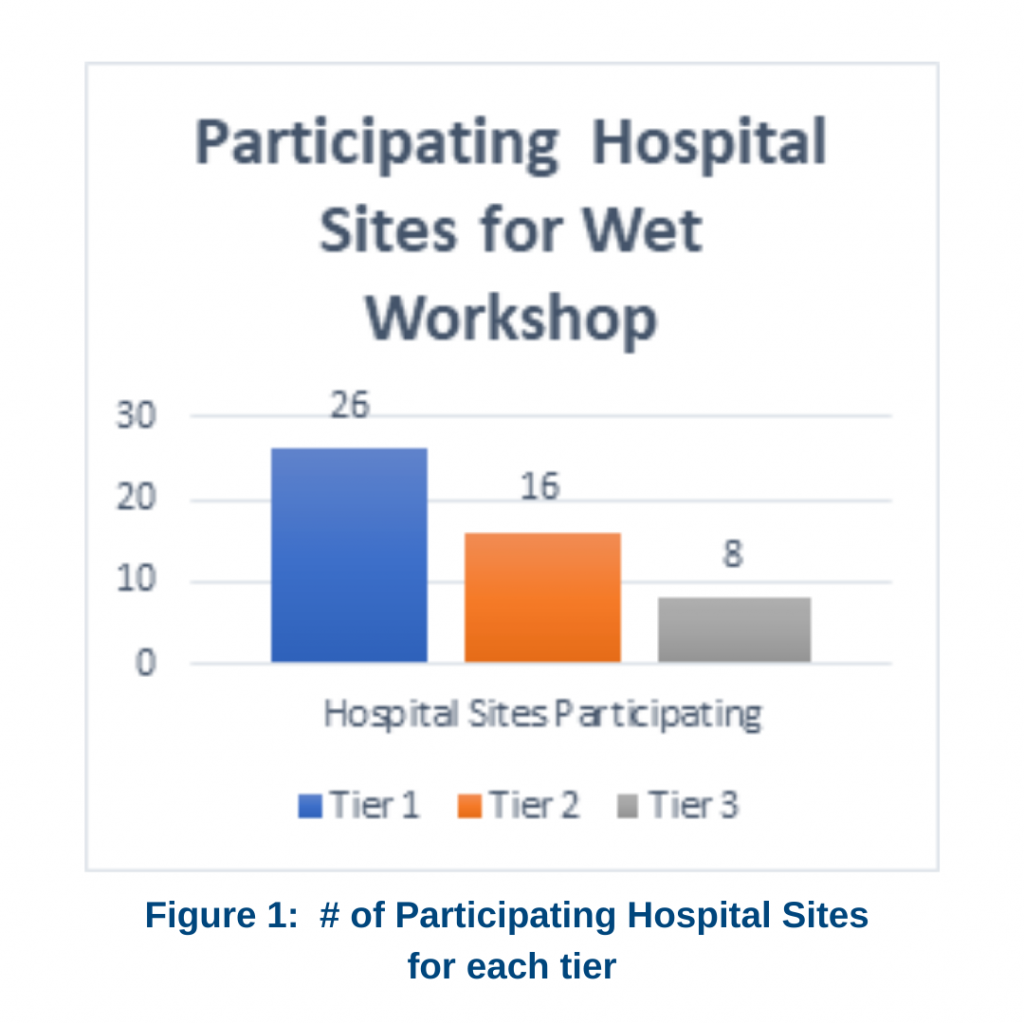
The testing was set up so a Tier 3 hospital would receive samples for all three levels, Tier 2 received samples for both Tier 1 and 2 and Tier 1 hospitals received only the samples for that level. The numbers of participating sites by Tier are illustrated in Figure 1.
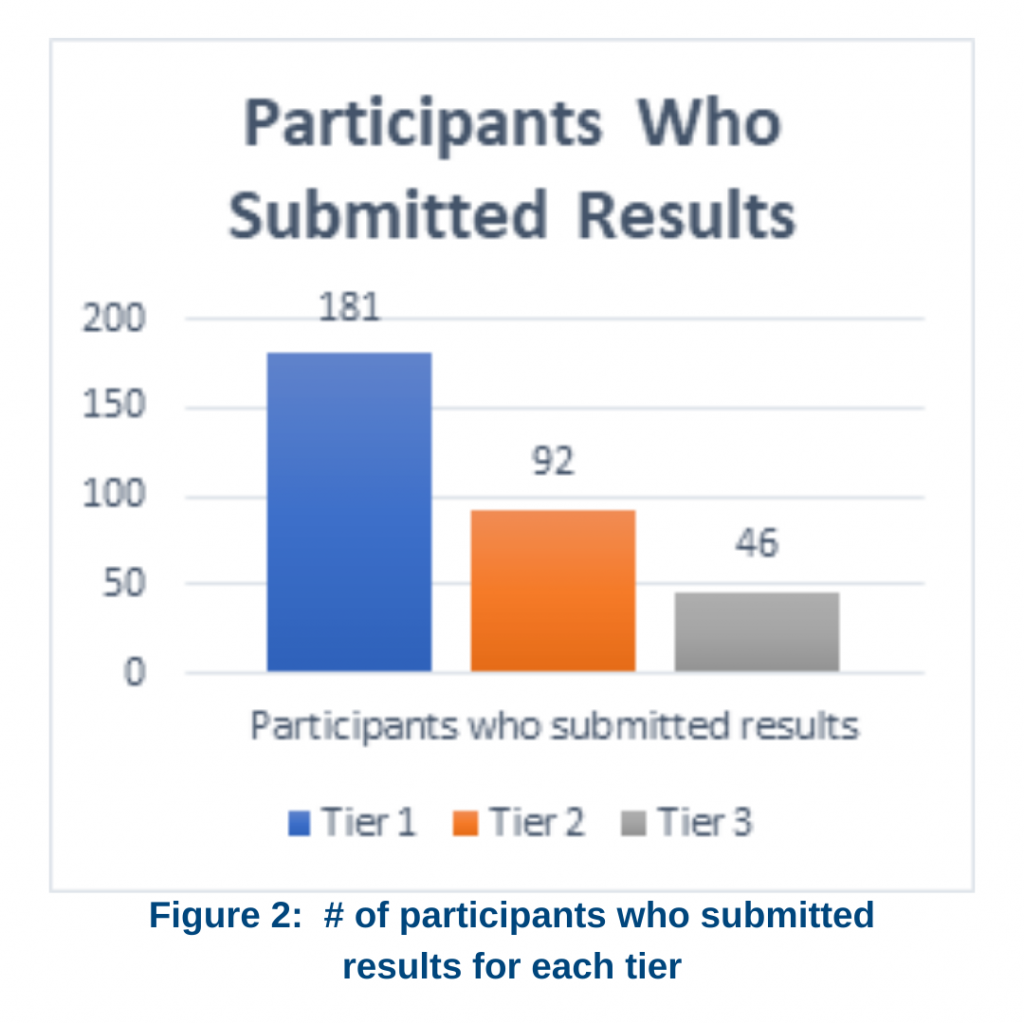
Hospital Technologists were given approximately 4 weeks to complete their testing and were sent a survey in which to enter their results. Figure 2 shows the number of participants that submitted results for each Tier. Following the completion date, the results of the survey were collated and a presentation was developed. On April 13th, three webinars were held to review the results and to discuss key learning points about the testing of these samples.
On April 14th, a virtual learning platform (GoToWebinar®) was used to stream four live presentations, once in the morning and once in the afternoon. The theme of these presentations was laboratory and clinical management of patients presenting with disease conditions for which transfusion is frequently required and the risk of alloimmunization is high. Transfusion experts provided both theoretical, evidence-based and practical guidance on how to best manage these patients.
The first presentation focused on the demographics and clinical care of patients with Sickle Cell Disease (SCD). These patients are becoming more numerous in Ontario and it was
recommended that hospitals across the province should be able to safely care for them. This talk, given by Dr. Jacob Pendergrast from the University Health Network, defined the principles of and indications for red cell transfusion for these patients, emphasizing the need for careful selection of red cells for transfusion and the importance of recognizing life-threatening hyperhemolysis.
The second presentation, by Dr. Yulia Lin from Sunnybrook HSC, focused on patients with Myelodysplastic Syndrome (MDS) and the approaches required to find appropriate blood products for them. Most patients with MDS become transfusion dependent, which is
associated with a decrease in survival rate and an overall decrease in quality of life. Dr. Lin shared information on transfusing MDS patients as outpatients and recognizing the lack of robust transfusion guidelines for this specific patient population.
The third presentation was given by the team of Ms. Melanie Tokessy and Dr. Johnathan Mack from the Eastern Ontario Regional Laboratory Association and The Ottawa Hospital. During the first half of the presentation Ms. Tokessy discussed how samples are processed in the lab to find the best matched product for patients with autoimmune hemolytic anemia.
She described the procedures for setting up the investigation and requirements for performing a crossmatch to find the most appropriate units for these patients. Dr. Mack discussed the indications for transfusion in this patient population and the reasons why physicians should be cautious when transfusing, but also the importance of not withholding transfusion in patients with life-threatening hemolysis. He described the reasons why response to transfusion should be monitored to guide therapy. He also provided some alternatives to blood transfusion in this group of patients.
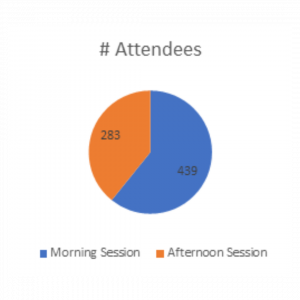
Preliminary attendance numbers are shown in Figure 3. Utilizing the GoToWebinar® platform worked very well, providing an easy way for participants to ask questions of the speakers. The sessions were recorded and are available for viewing on the www.transfusionontario.org website.
