October 2020

Alternatives to Transfusion
Why Transfuse Blood When You Can Make Your Own?
| The merits of iron over blood transfusion for treating iron deficiency anemia By Michelle P. Zeller MD FRCPC MHPE DRCPSC Case: A 24 year old woman sees her Family Physician (FP) because she has been more winded following her regular 5 km runs. Blood work shows her to be severely anemic and iron deficient. She is sent to the Emergency Department (ED) for urgent red blood cell (RBC) transfusion. This case is not an uncommon event. Patients like this present to their FP and to the ER often, though many of them are not capable of a 5 km run due to symptoms of iron deficiency anemia (IDA). Iron deficiency is the most common cause for anemia around the globe affecting most commonly women of reproductive potential and young children.1–3 Symptoms of iron deficiency with or without anemia vary from mild to severe and can include fatigue, irritability, decreased cognition, restless legs and hair loss. In severe cases of IDA, patients are at risk of epithelial tissue injury and chronic congestive heart failure/ Those with IDA in pregnancy are at additional risk of having low birth weight infants, preterm delivery and transfusion during pregnancy.1,4 Iron deficiency is not a diagnosis; it is a consequence. Once iron deficiency is identified (see Table 1) using biochemical and hematologic indices, the cause must be elucidated. |
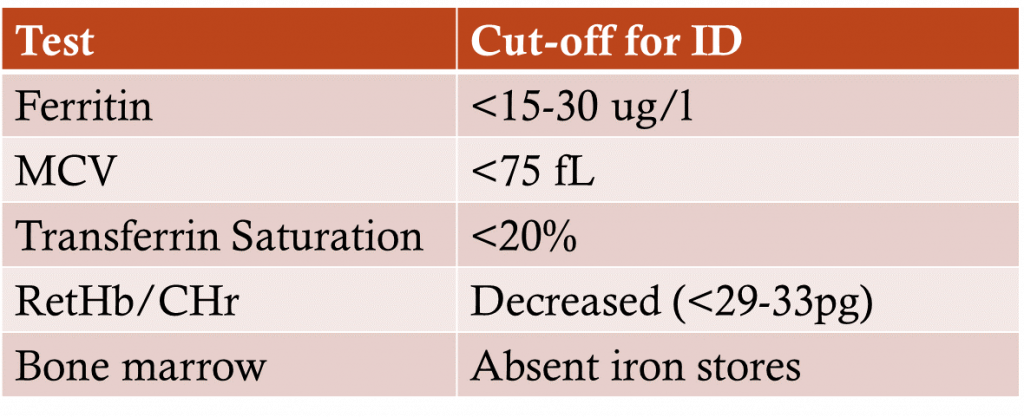
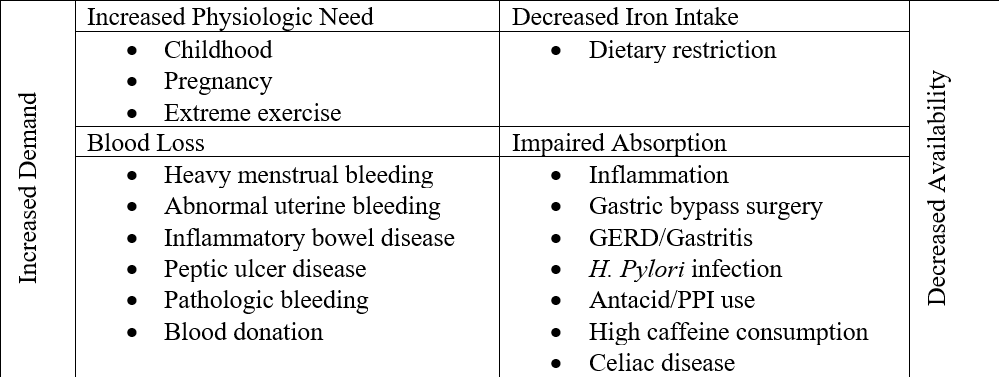
Identifying the etiology of IDA requires taking a clinical history and performing a physical examination that will direct laboratory and other diagnostic investigations. There are 4 major categories of causes (Table 2).6 Individuals may have multiple reasons for being iron deficient.
Management of iron deficiency consists of 2 parts:
- Treat/address the underlying etiology
- Iron repletion
The type and route of iron repletion depends on the severity, cause, comorbidities and preferences of the patient, the urgency of correction and resources available. Iron is commonly absorbed through diet and can be found in iron-fortified foods (certain cereals), meat, chicken, green leafy vegetables, and many other foods. Unfortunately, diet alone is often insufficient to replete iron deficiency.
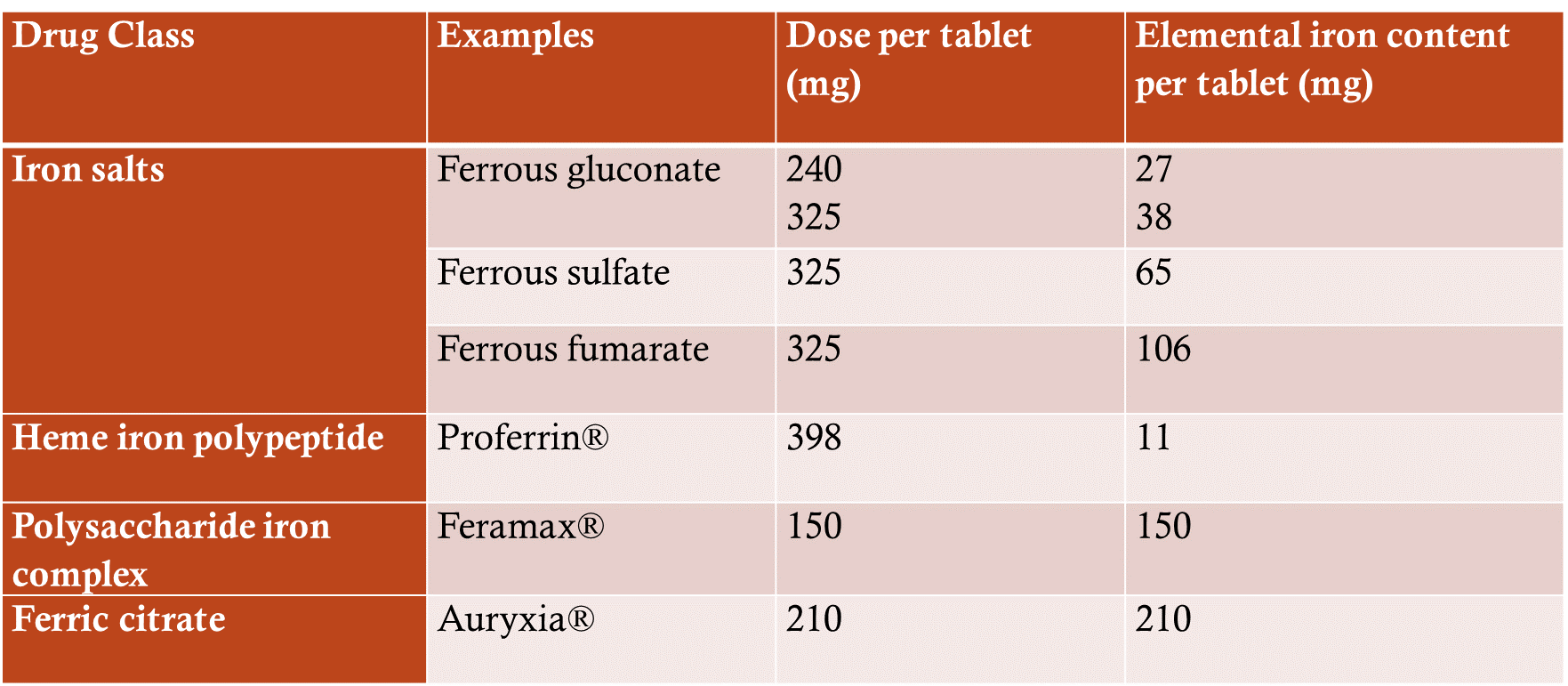
Oral iron supplements (Table 3) are widely available, often inexpensive and do not require a prescription. The downside to oral iron supplements is that they are sometimes poorly tolerated due to gastrointestinal side effects; and they will not work in every patient. Sometimes patients are unable to absorb iron through the oral route. They may be able to absorb small amounts with minimal side effects, but this may be insufficient to replete the degree of iron deficiency.
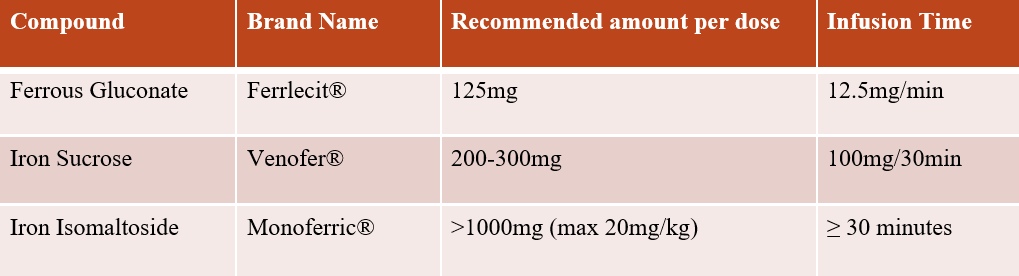
Intravenous (IV) iron has been available for decades and is both safe and effective.8–11 IV iron bypasses the GI tract and can deliver a large amount of iron over a relatively short period of time. Most patients tolerate IV iron without issue; however, some will experience nausea, headache, muscle aches and pains and/or fatigue around the time of infusion. The risk of severe anaphylactic reactions is rare. The cost of IV iron varies by formulation, and accessibility varies by institution. Table 4 summarizes the IV iron formulations available in Canada. A recent Canadian expert consensus provides guidance on managing hypersensitivity reactions to intravenous iron.12
There are many patient populations who benefit from IV iron including those with IDA secondary to inflammatory bower disease, heavy menstrual bleeding, abnormal uterine bleeding, pregnancy, gastric bypass surgery, systemic inflammatory diseases and those awaiting surgery.4,7,13–15 IV iron sucrose can be used safely in second and third trimester, but there is currently limited data on use of iron isomaltoside in any stage pregnancy, or use of iron sucrose in first trimester; these agents should be avoided or used with caution in pregnant women.
There is clear evidence that red blood cell transfusion should only be used as the last line of treatment for iron deficiency. This is emphasized by Choosing Wisely campaigns across specialties and jurisdiction: “Don’t transfuse red blood cells for iron deficiency without hemodynamic instability.” (AABB); “Don’t transfuse blood if other non-transfusion therapies or observation would be just as effective.” (Choosing Wisely Canada Transfusion Medicine).16–19 These statements recognize that the risk inherent in a unit of blood is greater than that in a dose of IV iron, and additionally consider patient preferences, resource allocation, and cost.
There are specific situations when transfusion of RBCs are necessary in the setting of IDA. Typically, such cases would include severe symptoms, ongoing and significant blood loss, and/or urgent need to optimize a patient’s blood supply due to their comorbidities.
How would we address the case presented above?
In a recent minireview on the role of IV iron in managing patients with IDA in the ED, 7 nonrandomized studies were identified.20 The studies showed benefit of IV iron over RBC transfusion on patient outcomes; however conclusions are limited by the observational study design, lack of controls, variable outcomes, risk of bias and low certainty of evidence. A conditional recommendation was made that considered the following:
- Prevalence, severity and sequelae of IDA,
- Risk of RBC transfusion,
- Safety, efficacy, feasibility of IV iron
- Resources and cost
- Acceptability to stakeholders
Conditional Recommendations: In the hemodynamically stable patient with IDA presenting to the ED, consider use of IV iron over RBC transfusion and use of IV iron over oral iron.20
Return to the case: The Emergency Physician recommended a dose of IV iron given the severity of the patient’s anemia. She felt that RBC transfusion was not required given the hemodynamic stability of the patient. She also referred the patient to gynecology for untreated heavy menstrual bleeding and recommended oral iron supplements and a follow up with the patient’s FP.
Acknowledgment: Thank you to Dr. Menaka Pai for reviewing & editing this article.
References:
Please view the PDF linked below for a full list of references.
View References
Using Blood Wisely – Will Your Hospital Take the Challenge?
By Doreen Day, Project Manager, Pan-Canadian Initiatives, Choosing Wisely Canada and Dr. Yulia Lin, Transfusion Medicine Specialist, Sunnybrook Health Sciences Centre & Transfusion Lead, Choosing Wisely Canada
Using Blood Wisely is a national campaign to decrease inappropriate red blood cell (RBC) transfusion practices in Canada launched by Choosing Wisely Canada in collaboration with Canadian Blood Services. Using Blood Wisely challenges hospitals to benchmark themselves on appropriate transfusion practices, supports hospitals wishing to embark on a quality improvement initiative to reduce inappropriate RBC transfusions, and recognizes hospitals who have already done great work in this area.
Using Blood Wisely has developed national benchmarks on transfusion appropriateness. These benchmarks are:
- At least 65% of red blood cell transfusion episodes are single unit transfusions
- At least 80% of inpatient red blood cell transfusions have a pre-transfusion Hb 80 g/L or less
These indicators were identified by the Using Blood Wisely Measurement Working Group as they have been recognized to be surrogate measures of appropriate red blood cell transfusion practice. These benchmarks were established based on audit data submitted by 21 participating hospitals to the Ontario Transfusion Quality Improvement Plan e-tracker tool where the 75th percentile for single unit transfusions was 67%. Similarly, the 75th percentile for inpatient pre-transfusion hemoglobin 80 g/L or less was 88%. Participating sites included a combination of 2 teaching and 19 community hospitals of various sizes. Data from the START study, which involved 13 hospitals (3 academic and 10 community sites) across 3 provinces, demonstrated a post-intervention result of 68% single unit transfusions and 85% pre-transfusion hemoglobin 80 g/L or less.
Will Your Hospital Take the Challenge?
Sign up and conduct a spot audit of red blood cell transfusion practice at your hospital by December 1, 2020 to see how your hospital compares to the benchmarks. Hospitals that exceed and maintain benchmarks will be eligible for the Using Blood Wisely Hospital designation from Choosing Wisely Canada and Canadian Blood Services. Hospitals that don’t meet the benchmarks are eligible to enrol in a quality improvement initiative where they will implement practices proven to reduce inappropriate transfusions and qualify for designation upon meeting the benchmarks. In addition, participation in this campaign will also be acknowledged as an organizational quality improvement initiative by Accreditation Canada’s Qmentum Program.
For more information, please visit www.usingbloodwisely.ca.
Upcoming Events:
October 22nd: University of Toronto Transfusion Medicine Rounds – Lessons from recent studies of platelet transfusions: what next?” presented by Dr. Simon Stanworth.

| October 30th: 15th Annual Transfusion Medicine Education Videoconference Symposium – Patients Are Not All the Same |
