February 2023
In This Issue
- The Elephant and Electric Touch: Er as the 44th Blood Group Antigen System
- A pathogen-reduced inventory at Canadian Blood Services with a focus on solvent detergent plasma
- Newsboard
- Tech assessment
- Register: Transfusionists Talk: Transfusion Made Bloody Easy
- Register: Provincial Bedside Audit of Blood Administration
- Upcoming Events
- UofT TM Round
The Elephant and Electric Touch: Er as the 44th Blood Group Antigen System
Dr. Christine M Cserti-Gazdewich,
Laboratory Medicine Program – UHN
The running joke is that our long and ever-expanding list of red cell surface antigens exists simply to create jobs for blood bankers. The transfusion of red blood cells (RBCs) might seem to be the easiest feat on Earth if it happens 100 million times annually, though what the ubiquitous act fails to reveal is just how much “behind-the-scenes” work goes in to compatibility- and safety- assurance. Likewise, 140 million babies are born every year, many with blood types different from the birthing parent. RBC rejection (in acute or delayed hemolytic reactions [HTRs], or in hemolytic disease of the fetus or newborn [HDFN]), occurs in less than 1 in every 1000 such encounters, giving the impression that human blood, in standard transfusion practice, mixes uneventfully enough. Those not as familiar with RBC surface marker diversity were therefore understandably surprised – despite Pandemic-driven enhancements in scientific literacy around antibodies, antigens, and “variants of concern” – to learn just how noisy and vulnerable the RBC can be in the crosshairs of the immune system. We do not just express the ABO system (with its four possible blood types [A, B, AB, and O]), or a D type in the Weiner system (“positive” [present] or “negative” [absent]). We express more than 40 other systems, which bear over 340 antigens within those formal bounds, with the possibility of “orphans” in so-called collections and series. Every act of transfusion or pregnancy permits us to see version-differences in shared molecules, or entirely different structures that we ourselves may lack, for an overall seroconversion rate of ~1-10%. The vast majority of the time, we can identify what these antibodies are, but sometimes we are left concluding “unidentified specificities,” with most but not all of these being insignificant.
The recent announcement1 on Er, the 44th system, was both a giant discovery and a re-shuffling of information in our ISBT tables.2 Three different Er antibodies were originally listed in the 200 series (“collection 208”), beginning with the high-prevalence anti-Er(a) in 1982, followed by the antithetical anti-Er(b), and then anti-Er3 (with mild HTRs) in Er(a-b-) individuals. What it took to go from a collection to a system was a series of proofs that these antibodies were targeting facets of a common molecule encoded by a specific gene with immunogenic variant loci. The Bristol group used state-of-the-art sequencing and gene-editing techniques to show that the PIEZO1 gene (on chromosome 16q24.3) – which encodes the Piezo1 mechanosensitive cation channel – was at the root. Piezo1 is an enormous (>2000 amino acid, >30 transmembrane pass) molecule that forms a propeller-like trimer or tetramer, permitting Na+ or Ca2+ (and thus water) influx with membrane pressurization. It is expressed across Kingdoms (from bacteria to mammals) and across tissues (from RBCs to endothelial cells and hollow organs [lungs, colon, kidneys, and bladder]). The discovery work behind this important class of master-sensors was recognized in the 2021 Nobel Prize.3
The Bristol team studied the expression and activity of this “electric touch” molecule further, and added two more antibodies to the list: anti-Er4 and anti-Er5, noteworthy for the sequelae of lethal HDFN.
Never miss out on the latest transfusion news and insights!
Sign up to our monthly newsletter; the ORBCoN Report.
Though the 13 other new systems identified in the last decade weren’t met with as much fanfare, several features set Er apart. Firstly, there are already five Er antibodies catalogued, and more expected, whereas 10 of the 13 other systems are marked by isoantibody formation alone in those lacking the carrier (ie- a presence vs absence situation, rather than alloimmunization fodder from what appears to be a highly polymorphic gene). Secondly, Er antibodies have occurred in people not from a single consanguineous founder group, but from places as far as Mexico, Germany, Kuwait, and Zimbabwe, ie- resisting the mold of other geoancestry-typical antibodies. Thirdly, a host of other Piezo1 mutations are known to produce disease states, such as the gain-of-function (slow de-activation) autosomal dominant mutation behind the malaria-protective state of dehydrated hereditary stomatocytosis (AD DHS), or the homozygous autosomal recessive loss-of-function state of generalized lymphatic dysplasia with non-immune hydrops fetalis. Knowing this molecule means knowing more about biology and disease. Fourthly, this molecule is present in a much lower membrane copy number than other RBC antigen systems, illustrating that target load is not a predictor of significance.
Though to us, the updated taxonomy on known and new antibodies does not change our practice overnight, a “system” status arguably earns a place of greater priority. For decades, disparate groups of biochemists and serologists saw only the separate parts of an elephant, and now the elephant is whole. Modern laboratory techniques may help shepherd the remaining orphan antigens into the systems of future news stories, and aid in the development of reference laboratory tools and more tailored blood inventories. Charged as we are with providing the right blood to the right patient, we now know more about why this might be hard in some rare cases, and how to go about getting the blood care mission accomplished.
References of Interest:
- The timeline: On Saturday September 24th 2022, the Bristol School of Biochemistry and the UK NHSBT’s International Blood Group Reference Laboratory (IBGRL) issued a press-release on the discovery of Er, the 44th blood group antigen system. The scientific paper was accepted for publication by Blood on Monday, August 15th and prepublished online a month later on Tuesday, September 20th. The story gained traction on social media and on evening news broadcasts around the world throughout the month of October 2022. (eg. https://toronto.citynews.ca/video/2022/10/16/scientists-discover-new-blood-group-er/)
The article came out in print as a Plenary Paper on Thursday January 12th 2023 (full reference:Karamatic Crew V, Tilley LA, Satchwell TJ, AlSubhi SA, Jones B, Spring FA, et al. Missense mutations in PIEZO1, which encodes the Piezo1 mechanosensor protein, define Er red blood cell antigens. Blood. 2023; 141(2):135-46.
https://doi.org/10.1182/blood.2022016504, PubMed PMID: 36122374), with an accompanying podcast: https://ashpublications.org/blood/pages/blood_podcast_s5ep2 - The ISBT’s Red Cell Immunogenetics and Blood Group Terminology Working Party’s website (https://www.isbtweb.org/isbt-working-parties/rcibgt.html) provides updated tables on antigens within the systems and collections (the 200 series [not meeting criteria for systems], and the subsets of the 700 series [low frequency antigens, <1%] and the 900 series [high frequency antigens, >99%]). Er now has its own listing: https://www.isbtweb.org/resource/044er.html
- The 2021 Nobel Prize in Physiology or Medicine: for David Julius and Ardem Patapoutian, and their discoveries of receptors for temperature and touch. https://www.nobelprize.org/prizes/medicine/2021/press-release/
A pathogen-reduced inventory at Canadian Blood Services with a focus on solvent detergent plasma
Kathryn Webert, MSc, MD, FRCPC
Medical Director and Special Advisor
Canadian Blood Services
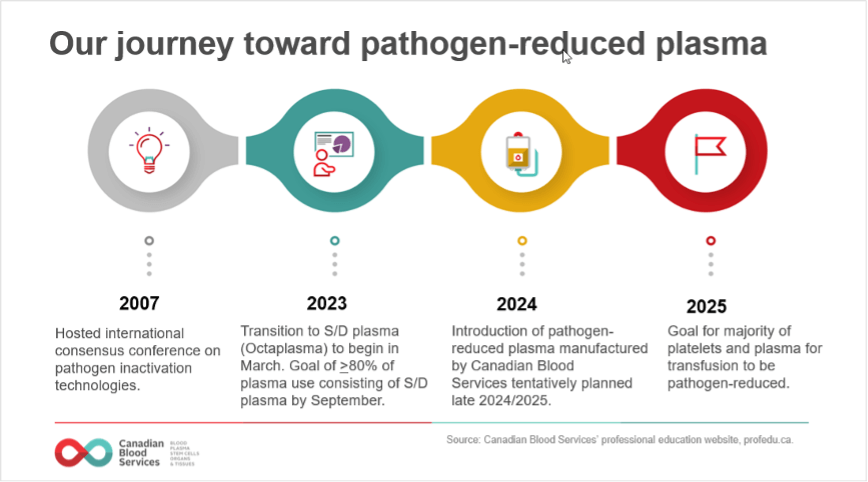
To provide an additional layer of product safety, Canadian Blood Services aims to introduce pathogen-reduced components and products, wherever possible (Figure 1). Our journey towards a pathogen-reduced inventory began in January 2022, when Canadian Blood Services began a staggered implementation of pathogen-reduced platelets.
In March 2023, the transition to pathogen-reduced plasma will begin with the widespread implementation of Octaplasma, a solvent detergent (S/D) treated plasma. In addition, implementation of another type of pathogen-reduced plasma, to be collected and manufactured by Canadian Blood Services using a different pathogen-inactivation technology and made available alongside S/D plasma, is tentatively planned for late 2024/25. Ultimately, it is expected that approximately 80% of plasma use will consist of S/D plasma and 20% will consist of Canadian Blood Services collected pathogen-reduced plasma. By 2025, the goal is for most platelets and plasma for transfusion to be pathogen-reduced.
Octaplasma is the commercial name for a pathogen-reduced form of frozen plasma manufactured by Octapharma. Octaplasma has been available only for special patient populations, but this will change as of March 2023, when it becomes available to all patients. Making it available to all patients is the most timely and cost-effective path towards a pathogen-reduced plasma supply.
Never miss out on the latest transfusion news and insights!
Sign up to our monthly newsletter; the ORBCoN Report.
When Octaplasma is manufactured, plasma from hundreds of donations is pooled. This step reduces antibodies that may be present in the plasma pool through dilution. The pooled plasma then undergoes sterile filtration steps resulting in the removal of leukocytes, as well as prions, parasites, and viruses. The plasma is treated with a combination of 1% tri(nbutyl)-phosphate, or TNBP, and 1% octoxynol. The detergent, octoxynol, interrupts the interactions between the molecules in viruses’ lipid coatings. Most enveloped viruses cannot exist without their lipid coating, so they are destroyed when exposed to these detergents. The solvent, TNBP, helps the reaction between the lipid coat and the detergent to happen more rapidly. The solvent and detergent reagents are removed by castor oil extraction (removes TNBP) and solid phase extraction (removes octoxynol). The plasma is then run through an affinity ligand resin column which specifically removes prion proteins. This step is considered effective for removing the infectious agent that causes variant Creutzfeldt-Jakob disease (vCJD) if present. The final product is packaged into blood bags with a standardized unit volume of 200 mL and frozen.
There are many benefits of S/D treatment: it reduces the residual risk of transfusion-transmitted infections that remain after donor screening and donation testing and reduces the risk of emerging or unknown pathogens that can be transmitted during transfusion to a patient. In addition, the literature suggests that S/D plasma may be associated with a decreased risk of adverse reactions, including allergic reactions and transfusion related acute lung injury (TRALI).1-5 The use of Octaplasma also benefits the blood system as it results in increased Canadian plasma available for fractionation.
On March 27, 2023, changes to the S/D plasma ordering process will be implemented, which will allow hospitals to order Octaplasma for all patients. By September 2023, all hospitals will be expected to order Octaplasma, with at least 80% of their plasma issues made up by Octaplasma by this date. This percent target will be guided by the experience of hospital customers as they transfuse more Octaplasma.
To assist hospitals during implementation steps, Canadian Blood Services is developing a series of educational materials which will be posted on our professional education website. Octapharma will also be making resources available.
Please contact Octapharma with any questions about Octaplasma and your local Hospital Liaison Specialist with any questions about Canadian Blood Services and plasma. Always refer to the Product Monograph for up-to-date information.6
References
- Saadah NH et al. Transition from fresh frozen plasma to solvent/detergent plasma in the Netherlands: comparing clinical use and transfusion reaction risks. Haematologica 105:1158-65 (2020).
- Liumbruno GM and Franchini M. Solvent/detergent plasma: pharmaceutical characteristics and clinical experience. J Thromb Thrombolysis 39:118-28 (2015).
- McGonigle AM et al. Solvent detergent treated pooled plasma and reduction of allergic transfusion reactions. Transfusion; 60:54-61 (2020).
- Klanderman RB et al. Reported transfusion-related acute lung injury associated with solvent/detergent plasma – A case series. Transfusion; 62: 594-99 (2022).
- Sachs UJ et al. White blood cell-reactive antibodies are undetectable in solvent/detergent plasma. Transfusion; 45:1628-1631 (2005).
- Octapharma. Octaplasma Product Monograph. October 21, 2022. Accessed at: https://www.octapharma.ca/en/therapies/product-overview
Newsboard
ORBCoN Tech Assessment

The ORBCoN Technologist Assessment program is now available on the new ORBCoN Learning Management System (LMS) and Surge Learning platforms.
A communication has been issued with instructions to provide site administrator information for access to the ORBCoN LMS and guidance for current Surge Learning clients.
If you have any questions or have not received the communication please reach out to alison.wendt@sunnybrook.ca
Provincial Bedside Audit of Blood Administration

Register: Transfusionists Talk: Transfusion Made Bloody Easy
Save the Date: 18th Annual TM Conference
Featured Resources
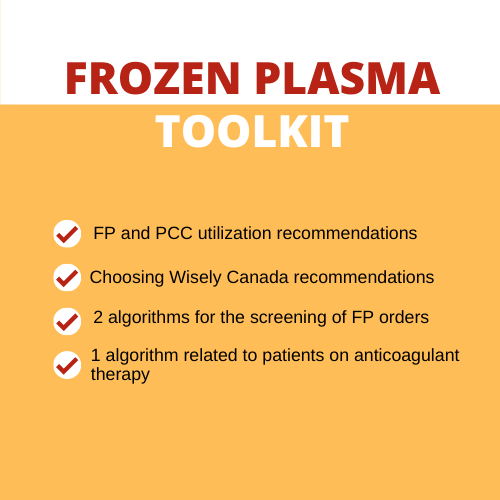
Frozen Plasma Toolkit
Upcoming Events
UofT TM Rounds

February 23, 2023 @12pm-1pm
ICTMG Behaviour change by Dr. Fabina Lorencatto & Dr. Justin Presseau